Pressure ulcer, Bedsores or Pressure ulcer is the destruction of the skin and underlying tissues. The deeper the wounds, the more difficult it is to heal. Pressure relief is the most important prevention and therapy of pressure ulcers.
What is bedsores (bedsores)?
.jpg)
© Alila Medical Media - stock.adobe.com
Decubitus (decubare, Latin: to lie) is what the doctor calls a chronic wound that is caused by mechanical overuse. Depending on the severity, the doctors differentiate between 4 stages of pressure ulcer.
In stage I of the pressure ulcer, a reddened area appears on the skin, which is often sharply demarcated. The redness does not go away spontaneously after pressure relief. In grade II decubitus ulcers, a blister has formed as the epidermis has become detached. In stage III of the pressure ulcer, the epidermis and subcutaneous tissue in the affected area have died (necrosis).
The connective tissue under the skin and muscles can also be affected by inflammatory processes. Doctors now speak of a pressure ulcer at the latest. Bare, inflamed bones mark the IV stage of the pressure ulcer.
causes
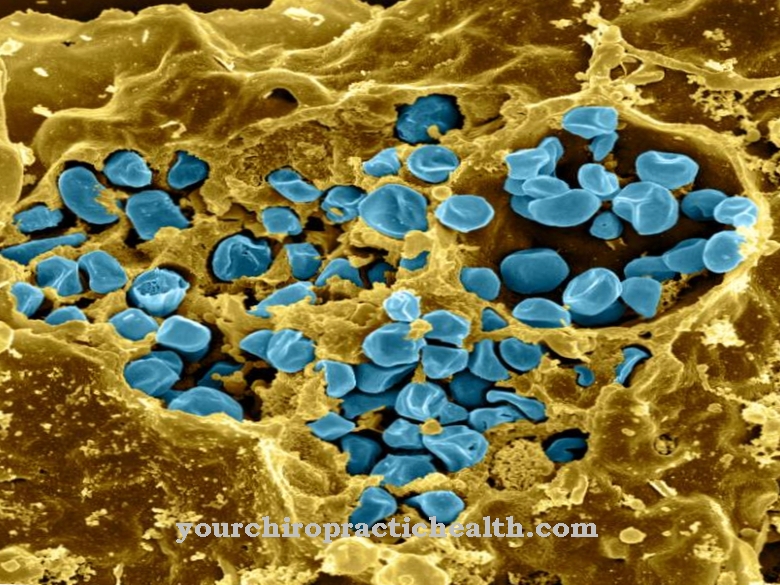
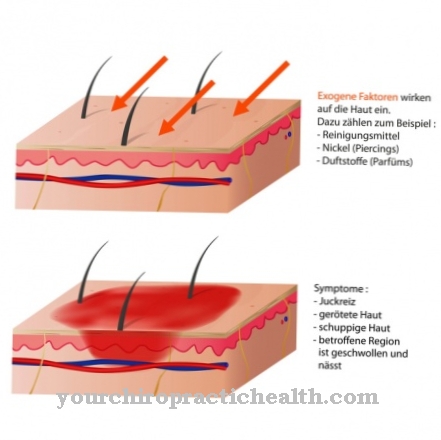
Pressure ulcers are caused by constant or regular strong pressure on the skin. The external pressure is greater than the blood pressure in the finest blood vessels (capillaries), which prevents blood flow. The insufficient supply of oxygen and nutrients to the skin causes it to die and inflammation of the dead tissue occurs.
This infection with pathogens spreads to tissue that is still healthy and leads to ulcer-like deep holes. Because excessive external pressure is the cause of the pressure ulcer, bedridden patients are affected in most cases.
But also overweight people with sedentary activities or disabled people in wheelchairs are risk groups. The pressure ulcer is localized in exposed parts of the body where the bone is not padded with connective tissue or muscles. The sacrum, hips, shoulders, heels and elbows are therefore the most common areas of pressure ulcer.
Symptoms, ailments & signs
The symptoms of a pressure ulcer show up in changes in the appearance of the skin. The course of the disease is divided into four stages, some of which are accompanied by great pain.
Grade 1: The first sign of a pressure ulcer is reddening of the skin, which persists even when the pressure is relieved. If you press the reddened area with your finger and it does not turn whitish, but remains red, the bedsore has reached the first degree. In addition, a slight swelling or hardening and warmth can be felt on the affected skin area.
Grade 2: As the pressure sore develops, it gradually penetrates deeper into the skin. The second-degree pressure ulcer is recognizable as a flat ulcer. Abrasions or blisters will form on the affected area. The damage can still be seen in the surface area of the skin, namely in the epidermis (upper skin) and parts of the dermis (dermis).
Grade 3: The pressure ulcer extends into the subcutaneous tissue and the underlying tissue is irreversibly affected. At this stage there is an open deep wound. If there is a germ infestation, putrid smells also occur.
Grade 4: The pressure ulcer extends to the muscles, bones and tendons. This tissue is also destroyed. Those affected suffer from enormous pain.
Diagnosis & course
Diagnosing pressure ulcers is primarily a matter of observation. A visual inspection should focus on the particularly endangered parts of the body. Even a layperson can recognize pressure ulcers in the early stages by means of red skin spots. Even a grade II pressure ulcer is so obvious that nobody can miss it.
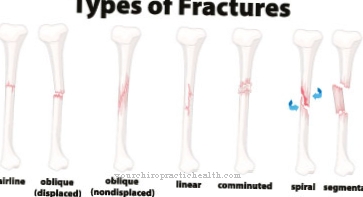
Of course, the doctor will take a smear from the wound to initiate the correct treatment. The question of the pathogens involved plays a decisive role for the chosen means. In the case of a very deep pressure ulcer, an X-ray can be useful to assess the exact extent of the tissue damage. The healing of a pressure ulcer is usually a very tedious process because it is an inflammatory and necrotic process.
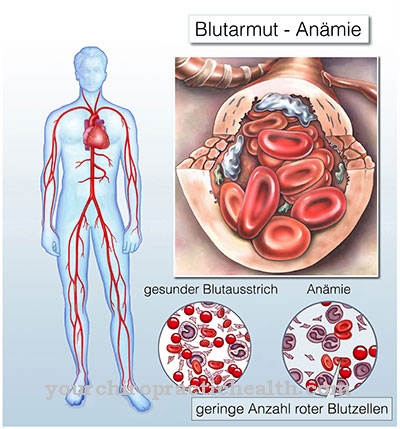
The tendency of pressure ulcers to eat deeper and deeper is particularly serious. The open, bacterially infected part of the body always means the risk of an overarching infection. Blood poisoning from pressure ulcers is a risk that must always be taken into account. Inflammation of the bone marrow can also result from the pressure ulcer, and even the pathogens causing pneumonia make their way through the gaping pressure ulcer.
Finally, pain and the knowledge of an open and deep wound also lead to mental disorders. Depression and apathy are often also the result of pressure ulcers.
When should you go to the doctor?
A pressure ulcer is a serious wound that needs professional care. The basis of all things is to take suitable measures to prevent pressure ulcers. If a pressure sore has nevertheless developed, a nurse must be called in as a minimum.
It is not advisable for family caregivers to take action in the event of a pressure ulcer without the guidance of a doctor. A pressure sore always requires professional treatment. At the same time, before the pressure ulcer heals, improved measures must be taken to prevent bedsores from recurring. Special anti-decubitus mattresses prevent pressure sores from forming in bedridden patients.
The wound care is based on the type and severity of the pressure ulcer. Small and dry pressure sores can be loosely covered with sterile bandages. Weeping pressure ulcer wounds must first be cleaned with sterile saline solution. Then an airtight hydrocolloid dressing can be applied. This keeps the wound moist. The weeping pressure ulcer can heal without sticking to the plaster bandage.
With an advanced pressure ulcer, dead tissue becomes a problem. A doctor must remove this, observing sterility. Wound cleaning is time-consuming. It is carried out in several phases. It is necessary to have wound swabs regularly to rule out infection. Treatment with antibiotics may be unavoidable. Particularly deep pressure ulcer injuries require hospitalization and surgical intervention.
Doctors & therapists in your area
Treatment & Therapy
Treating bedsores means first of all to relieve pressure. A bedridden patient is not only allowed to lie on his back, but must be repositioned every 2 hours, around the clock. This is done according to a set plan that is designed so that the patient does not lie on one side of the body too often.
The carers use positioning aids in the form of anatomically adapted pillows to give the patient the necessary support in bed. Special bedsore mattresses adapt to the shape of the body and distribute the pressure more evenly when they are placed on them.
Water beds are particularly effective in the same way against pressure ulcers, as are water pillows that can be pulled in under the sheet. Treatment of wounds in pressure ulcers by rinsing with potassium chloride solution or hydrogen peroxide aims to combat the infection.
Preparations in powder form such as silver nitrate also counteract the inflammation. The doctor surgically removes dead tissue and thus also removes a large part of the bacteria involved. If the inflammation spreads across the board, oral antibiotics are essential therapy for pressure ulcers.
Outlook & forecast
The healing of the pressure ulcer depends on various influencing factors. The stage of the sore spots as well as the underlying disease and the age of the patient are the most important criteria in making a diagnosis. The sooner a pressure ulcer is recognized and treated, the better the chances of recovery. If there is a possibility that the underlying disease will heal, the patient is no longer dependent on being bedridden. In these cases, the sore spots usually heal completely within a few weeks.
If the person concerned is confined to bed or sitting in a wheelchair, the prognosis worsens. A cure is still possible. At the same time, however, the risk of developing pressure ulcers again after recovery increases. Poor wound healing leads to further deterioration in health in most cases without treatment.
If the outcome is unfavorable, secondary diseases set in that lead to long-term treatment or permanent damage. If germs penetrate the wounds, there is a risk of blood poisoning. If the conditions are poor, the patient may die prematurely.
Older people naturally have less wound healing properties. Under certain circumstances, the pressure ulcer may not heal despite medical care. These patients experience a chronic course of the disease.
prevention
Preventing pressure ulcers by relieving pressure has long become standard in modern care. In addition to repositioning the bedridden and positioning aids, skin care measures are an important point. Special oils and emulsions help keep the skin healthy, and products that promote blood circulation such as rubbing alcohol should be used daily. If possible, caregivers should mobilize the patient gradually. After all, these activating care measures are not just a prevention of bedsores.
Aftercare
After a pressure ulcer has healed, the affected area should be adequately followed up. In consultation with the treating physician, nourishing creams, hygiene measures and care for the wound or scar area should be applied. In addition, care should be taken to protect the skin and the surrounding soft tissues, both for follow-up care and to protect against further bedsores. This is especially true for places that are mechanically particularly stressed.
For example, shoes that are too tight should not be worn and lying in one position for too long should be avoided if possible. Here, for example, cushioning cushions can be placed under the heels. For chronically bedridden patients, it is advisable to change the lying position several times a day and to support them with soft blankets or pillows.
A doctor's prescription for a pressure ulcer mattress, which inflates electrically to reduce the contact pressure, is also useful here. For prevention, existing diseases such as diabetes or circulatory disorders should be stopped and controlled with medication.
This is also important if patients tend to have decubitus sores that have not yet completely healed, as underlying diseases promote wound healing disorders and bacterial infections. If individually possible, weight reduction should be aimed for, especially in overweight patients. It is also important to ensure that you drink enough water.
You can do that yourself
The measures that those affected by a pressure ulcer can take themselves to treat or even prevent a corresponding wound depend on their degree of mobility and their ability to properly perceive the affected parts of the body.
The first priority for those affected is communication with relatives or caregivers. Even if a pressure ulcer is suspected or irritation is felt in an inaccessible part of the body, a control should be urgently requested.
Hygiene measures are also relevant and must be implemented. Affected parts of the body need to be washed, especially after a bowel movement or urination. Otherwise, the risk of pressure ulcers increases or an existing wound is further irritated.
The diet should be rich in vitamins and minerals to strengthen the skin. Sufficient fluids are also recommended. Massages of little-moved or otherwise endangered parts of the body also help. Substances that stimulate blood circulation are particularly suitable as massage oils. Rosemary or peppermint come into consideration here.
In areas that have already been affected, it is important that there are no pressure points during storage. Hoses, folds from clothing or bed linen and the like must be removed or avoided. Clothing that is too tight should also be avoided.
Marigold ointments are suitable as a support for wound care. The possibilities for self-help are very much dependent on the other clinical picture. Affected people who have very limited mobility should not be afraid of communicating about hygiene and other measures.



.jpg)











.jpg)