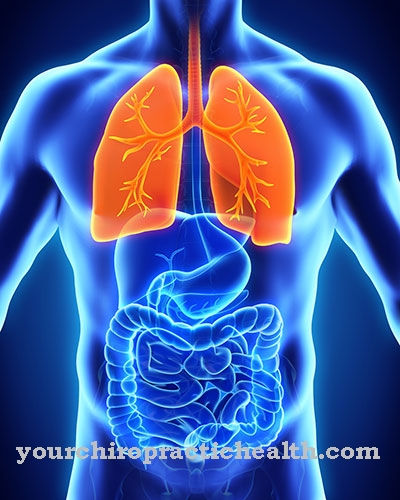
Under distribution one understands the uneven distribution of ventilation (ventilation of the lungs), perfusion (blood flow to the lungs) and diffusion (gas exchange). This also reduces the arterialization of the blood in healthy people. Arterialization describes the setting of the arterial respiratory gas partial pressures.
What is the distribution?

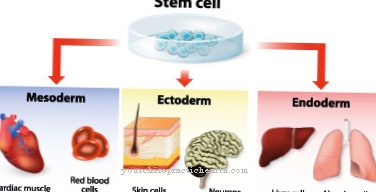
Humans are dependent on a constant supply of oxygen. The removal of metabolic products, especially carbon dioxide, is just as important. This gas exchange takes place in the lungs, more precisely in the alveoli (alveoli) and is known as ventilation. The ventilation determines how much oxygen gets into the alveoli and how much carbon dioxide is removed from them.
The oxygen reaches the tissues where it is needed via the bloodstream. The carbon dioxide as a metabolic end product also reaches the lungs via the bloodstream, where it is exhaled. This blood flow is called perfusion. The ventilation-perfusion ratio is of central importance when setting the arterial partial pressures of the breathing gases.
The third factor, which does not affect the arterialization of the blood as much, is diffusion. Diffusion is understood as the passage of respiratory gases through the alveolar wall. According to Fick's law of diffusion, it is dependent on the partial pressures of the breathing gases, the diffusion distance and the available area.
The distribution results from these 3 factors.
Function & task
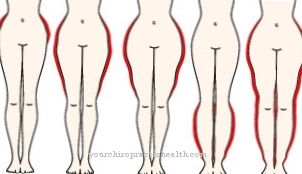
The lungs are not a homogeneous organ, which means that not all areas are equally well supplied with blood and ventilated. Physiologically it is the case that the lower lung areas are better ventilated and perfused than the upper ones. There is also a small portion (2%) of the blood volume that is bypassed by the gas exchange areas. This blood is called shunt blood. It remains low in oxygen and goes straight to the arterial system. As a result, the oxygen partial pressure is reduced here. If two lung areas are now ventilated differently, then the well arterialized blood from the more strongly ventilated area is constantly mixed with poorly arterialized blood from the less ventilated area. This results in a mixture in which the O2 partial pressure is lower and the CO2 partial pressure is somewhat higher.
Due to the irregular distribution of ventilation, perfusion and diffusion and the additional admixture of shunt blood, there is less oxygen in the arterial blood than in the alveoli. A statement about the overall effect of breathing can be made using the level of the arterial partial pressures.
The lung function is measured using these parameters.The arterial oxygen partial pressure decreases with age, which can be attributed to an increase in distribution irregularities. R.
Typical values for the arterial oxygen partial pressure are approx. 95 mmHg in healthy adolescents, 80 mmHg in a 40-year-old and 70 mmHg in a 70-year-old. However, the partial pressure drop has only a minor influence on the actual O2 saturation of the hemoglobin. This is because the O2 binding curve has a very flat profile in the higher partial pressure range. This means that in adolescence, O2 saturation is around 97% and this value is only reduced to around 94% in older people. This ensures that the blood is adequately oxygenated even in old age.
You can find your medication here
➔ Medication for shortness of breath and lung problemsIllnesses & ailments
In the case of lung diseases, the arterialization is all the more diminished due to deteriorated distribution. All diseases that affect ventilation, perfusion and diffusion ultimately affect the setting of the arterial respiratory gas partial pressures. The result is almost always a decrease in the oxygen partial pressure with a simultaneous increase in the carbon dioxide partial pressure.
Above all, however, the arterialization effect is determined by the ratio of ventilation to perfusion. Physiologically, this value is 0.8-1. If it is below this, it is a matter of hypoventilation. All values above are called hyperventilation.
With alveolar hypoventilation, the O2 partial pressure falls and at the same time the CO2 partial pressure rises to the same extent. This change is also shown in the blood and hypoxia occurs. As a result, the hemoglobin load of oxygen is greatly reduced and cyanosis occurs. Cyanosis is the bluish discoloration of the skin.
Alveolar hyperventilation is associated with an increase in O2 and a decrease in CO2. However, the organs are not supplied with improved oxygen, since the hemoglobin is already maximally saturated under normal conditions. However, the cerebral blood flow can be reduced by the drop in carbon dioxide.
One type of ventilation disorder is called atelectasis. There is insufficient ventilation of sections of the lungs. This is caused, for example, by the obstruction of a bronchus. The consequence is a deterioration in oxygenation. In addition, a pleural effusion or a pneumothorax can impair ventilation and thus worsen distribution. Pleural effusion is caused by an accumulation of fluid and in pneumothorax an accumulation of air is the cause.
Obstructive ventilation disorders are associated with constriction of the bronchi. This reduces the ventilation of the lungs. Examples of this are bronchial asthma or chronic obstructive pulmonary disease.
The most common perfusion disorder is pulmonary embolism. By spreading a thrombus, a pulmonary artery closes and the lungs are no longer supplied with blood. The body tries to compensate for this by increasing the heart rate. Dyspnea also occurs.
Diffusion can also be disturbed, for example by pulmonary edema. The patient notices the worsened distribution mainly because of the pronounced shortness of breath.










.jpg)

.jpg)