In the Erdheim-Chester disease it is a so-called non-Langerhans type of histiocytosis. This is a multi-system disease that is associated, for example, with skeletal complaints or pain in the bones or diabetes insipidus. In addition, damage to the kidneys and the central nervous system in connection with cardiovascular symptoms is possible. Erdheim-Chester disease is often referred to by the abbreviation ECD.
What is Erdheim-Chester Disease?

© staras - stock.adobe.com
Erdheim-Chester disease is an extremely rare form of histiocytosis. In the history of medicine since 1930, only about 500 cases of ECD are known. Less than 15 cases occurred in childhood. On average, those affected are 53 years old when the disease begins.
However, there is no familial accumulation of the disease, so that, based on current knowledge, it is not assumed that Erdheim-Chester disease is inherited. The ECD was discovered at the beginning of the 20th century by Jakob Erdheim, an Austrian pathologist. At the time of discovery, Erdheim was doing a research stay in Vienna. The disease was first described in 1930 by the British heart disease doctor William Chester.
causes
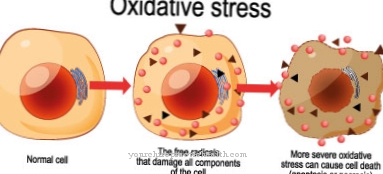
According to the current state of medical research, the causes for the development of Erdheim-Chester disease are not yet known. However, both reactive and neoplastic causes are under discussion as potential causes of the disease. In patients suffering from Erdheim-Chester disease, increased levels of interleukin, interferon-alpha and monocyte chemoattractive protein 1 were found.
At the same time, decreased levels of IL-4 have been shown. Overall, the findings indicate that the disease is a systemic and Th-1-oriented immune disorder. In addition, mutations in the BRAF proto-oncogene were found in over half of the affected patients examined. This gives another indication that the causes of Erdheim-Chester disease are very complex.
You can find your medication here
➔ Medicines for painSymptoms, ailments & signs
The possible symptoms and complaints that can occur in connection with Erdheim-Chester disease are very diverse. In general, several organ systems are affected by the disease in ECD, so that the symptoms are very different depending on the severity. In about half of the cases, the affected patients suffer from complaints of the skeletal system.
The most common symptoms are pain in the bones in connection with symmetrical osteosclerotic changes in the long tubular bones. Symptoms of the retroperitoneal space, the lungs and the kidneys were also observed. In most cases, Erdheim-Chester disease begins in adulthood between the ages of 40 and 60.
The disease occurs three times as often in men as in women. The course varies greatly depending on the patient and the severity of the disease. In some cases, especially at the onset of the disease, there are no symptoms at all. In severe cases, however, the symptoms are multisystem and become life-threatening. One of the characteristics of ECD is osteosclerosis, which occurs on the long tubular bones.
This leads to bone pain, which particularly affects the lower extremities. If the pituitary gland is infiltrated as part of the disease, diabetes insipidus usually follows. A deficiency of gonadotropin and hyperprolactinemia are also possible less frequently. General symptoms of Erdheim-Chester disease are severe weight loss and feelings of weakness.
Infiltrating other organs can lead to increased intracranial pressure, papillary edema, exophthalmos, or adrenal insufficiency. If the central nervous system is involved, headaches, cognitive impairments and seizures are possible.
Sensory disorders and paralysis of the cranial nerves can also occur. In addition, cardiovascular changes such as the so-called coated aorta often develop as part of the ECD.
diagnosis
Erdheim-Chester disease is diagnosed on the basis of a combination of typical symptoms that do not occur in this form in other diseases. If, in the course of histological examinations, xantho-granulomatous or xanthomatous tissue infiltration in connection with histiocytic foam cells, the diagnosis of the ECD is considered confirmed.
On x-rays, symmetrical and bilateral cortical osteosclerosis on the long tubular bones indicates the disease. If an abdominal CT scan is performed, around half of the affected people will show a so-called hairy kidney. In this case, a biopsy is recommended. As part of the differential diagnosis, for example, histiocytoses in Langerhans cells, Takayasu arteritis and primary hypophysitis must be excluded.
When should you go to the doctor?
Persistent pain in the bones and joints should be examined and treated by a doctor. If the pain spreads across the body or if it intensifies, a doctor is needed. Before taking any pain reliever medication, you should consult a doctor so that risks and side effects can be discussed and clarified. If the complaints lead to a bad posture of the body or one-sided stress, a doctor's visit is necessary.
Without a correction there is a risk of permanent damage to the skeletal system. Disorders of movement coordination and unsteady gait should be discussed with a doctor. In the event of unplanned and unexpected weight loss or general weakness, a doctor should be consulted. Cramps, headaches or reduced performance are considered worrying if they persist over several days.
If you experience concentration problems or repeated attention deficits, you should consult a doctor. Symptoms in the kidney region are considered unusual and should be clarified by a doctor if they have persisted for several days. Changes in urine or problems urinating should be discussed with a doctor. If you have a fever, a feeling of illness or functional disorders of individual systems, a doctor should be consulted. If skin changes or structural changes in the bones are noticed, this is also cause for concern and a doctor should be consulted.
Doctors & therapists in your area
Treatment & Therapy
In the therapy of Erdheim-Chester disease, steroids and cyclophosphamide as well as bisphosphonates and etoposide are used. The bisphosphonates in particular are able to reduce the pain in the bones. The use of vemurafenib and infliximab, which have already shown some success against ECD, is currently being investigated.
The chances of recovery and prognosis for Erdheim-Chester disease depend on the severity of the disease and the degree to which the internal organs are affected. If the therapy is ineffective, the majority of patients will die of pneumonia, congestive heart failure or kidney failure approximately two to three years after the diagnosis has been made. Basically, life expectancy depends on how badly the organs are damaged.
Outlook & forecast
Erdheim-Chester disease is one of the extremely rare diseases. The causes of the disease are unclear. Around 500 people are affected worldwide. Erdheim-Chester disease leads to a concentration of specific symptoms. It depends on the severity of the symptoms and the resulting organ damage which prognosis is given for the person concerned.
The consequences of Erdheim-Chester disease are usually severe. Several organ systems are affected by damage and disease consequences. Depending on the degree of damage, quality of life and life expectancy can be reduced to a greater or lesser extent. Medical advances toward healing can be made in the milder forms. The advances are based on drug treatment.
What is difficult is that Erdheim-Chester disease, as a multi-system disease, has so many aspects. In sum, these often result in a severe clinical picture. This is difficult to deal with in its individual components. The prognosis for Erdheim-Chester disease can therefore be very different. In general, if the central nervous system is involved, the prognosis is worse.
Patients used to survive Erdheim-Chester disease by only one and a half years. Thanks to modern treatment approaches, this period has now been extended. A quarter of those affected die within 19 months of being diagnosed. Almost 70 percent of those affected will now survive the next five years. However, you are dealing with severe symptoms.
You can find your medication here
➔ Medicines for painprevention
Since Erdheim-Chester disease has not yet been adequately researched, there are no known effective methods of preventing the disease. A doctor should be consulted immediately at the first signs of the disease.
Aftercare
Erdheim-Chester disease, which is very rare, usually occurs after the age of fifty. In even rarer cases it can be found in children and adolescents. A gene mutation is assumed to be the cause of the disease - and this makes follow-up care difficult. It cannot currently aim at recovery, but only at alleviating and monitoring the many symptoms.
Since organ damage can occur in the course of the disease, which varies in severity, the frequency of care depends on the course of the disease. These include severe bone pain and bone changes, fever, diabetes insipidus, severe weight loss, organ damage or damage to the CNS. Therefore, Erdheim-Chester disease is a multi-system disease.
Medical follow-up care for Erdheim-Chester disease should ensure the highest possible quality of life. This is largely only possible through the administration of medication. These can have severe side effects. Treatment is also difficult because of the rarity of Erdheim-Chester disease. Without treatment, however, the tissue, including the organs, becomes fibrotic. There is a risk of failure of the affected organs.
Long-term administration of antibiotics or other preparations can be helpful in aftercare. Physical therapies or occupational therapy are also helpful, as well as speech or swallowing therapy for appropriate indications. Sometimes those affected are dependent on a wheelchair.
You can do that yourself
Erdheim-Chester disease (ECD) is a multisystem disease with skeletal symptoms. The disease is very rare and its causes have so far hardly been researched. So the patient cannot take any measures that have a causal effect. The best contribution to self-help is to identify the disorder as early as possible and have it treated. The prognosis for the course of the disease and the patient's chances of survival depend heavily on which organs are already affected at the start of treatment and how far the damage has progressed.
The symptoms and clinical picture of ECD are extremely heterogeneous and depend on which organs are affected. People with multiple organ disorders should consult a doctor promptly, even if the symptoms seem harmless at first and seem to subside again. Patients themselves cannot contribute much to the treatment of ECD, but they can discontinue counterproductive behavior.
Pneumonia is a common side effect of ECD. Those affected should therefore not unnecessarily strain the lungs and, in particular, stop smoking. A healthy lifestyle that improves general wellbeing and strengthens the immune system supports the medically prescribed therapy and increases the chances of recovery.

.jpg)

.jpg)