The Fibrinolysis is characterized by the dissolution of fibrin by the enzyme plasmin. It is subject to complicated regulatory mechanisms in the organism and is in balance with hemostasis (blood clotting). A disturbance of this balance can lead to severe bleeding or thrombosis as well as embolism.
What is fibrinolysis?

The term fibrinolysis refers to the enzymatic breakdown of fibrin. Fibrin is a protein that is insoluble in water and plays a major role in blood clotting. It represents a cross-linked system made up of several polypeptide chains. The cross-connections between the individual polypeptide chains are formed via covalent peptide bonds.
As the main component of blood clots (thrombosis), fibrin is responsible for their stability. During fibrinolysis, the cross-connections of the network are broken, resulting in water-soluble fragments. These fragments are then transported away via the blood stream.
In the case of injuries, hemostasis (blood clotting) always occurs first, so that the bleeding is stopped. However, hemostasis also immediately activates fibrinolysis. When the process of wound healing is complete, the balance shifts in favor of fibrinolysis.
Function & task
The function of fibrinolysis is to limit the process of blood clotting in injuries. Otherwise, hemostasis would continue until the injured blood vessel was blocked. The result would be a thrombosis, which could easily lead to a fatal embolism.
The wound healing process thus takes place within the framework of a precisely coordinated balance between thrombus formation and thrombus breakdown. Fibrinolysis can be activated or inhibited. At the same time, however, the activation of fibrinolysis can also be inhibited.
Hemostasis is also controlled by activating and inhibiting processes. This complicated balance ensures an undisturbed wound healing process.
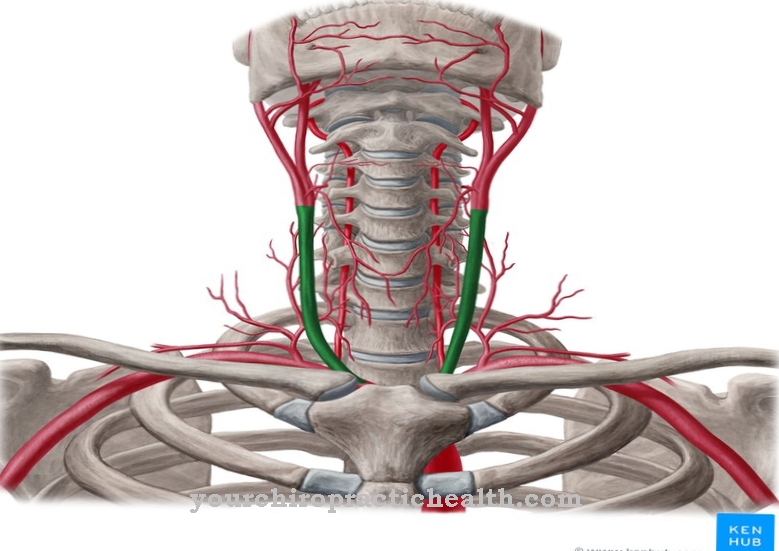
Both endogenous and exogenous enzymes can be used to activate fibrinolysis. The body's own activators of fibrinolysis include the tissue-specific plasminogen activator (tPA) and urokinase (uPA).
Foreign activator enzymes are produced by staphylococci and streptococci. The tissue-specific plasmininactivator comes from the endothelial cells of the vessel wall. Its release is initiated somewhat delayed by activating the plasmatic coagulation system via a complicated control mechanism.
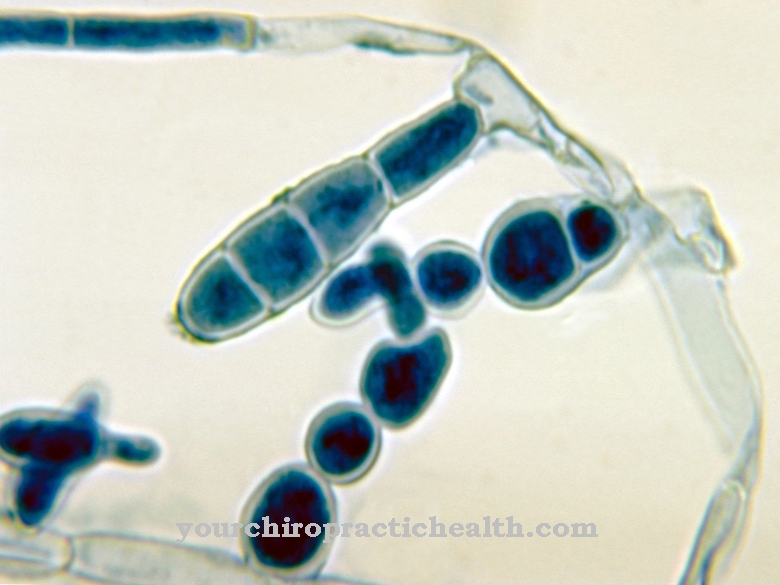
The tissue-specific plasmin activator is a serine protease that controls the conversion of plasminogen into plasmin. Plasmin, in turn, is the actual fibrin-degrading enzyme. The other endogenous fibrinolysis activator urokinase (uPA) also converts plasminogen into plasmin. Urokinase was first discovered in human urine. The fibrinolysis activators staphylokinase and streptokinase are produced by the corresponding bacterial strains and also convert plasminogen into plasmin. The haemolytic effect here leads to a further spread of the infection.
However, all four enzymes are also used as active ingredients in drugs for the treatment of thrombosis. The plasmin formed has the task of breaking down fibrin. The thrombus then dissolves. In order to limit fibrinolysis, however, both inhibitors of fibrinolysis activation and direct plasmin inhibitors are formed in the organism.
To date, four different inhibitors of fibrinolysis activators have been discovered. They all belong to the Serpine family and are referred to as PAI-1 to PAI-4 (plasminogen activator inhibitor). These inhibitors are stored in the platelets. When the platelets are activated, they are released and in turn inhibit the fibrinolysis activators.
Plasmin can also be inhibited directly. This is mainly done by the enzyme alpha-2-antiplasmin. During blood clotting, this enzyme is cross-linked with the fibrin polymers so that the thrombus is stabilized against fibrinolysis. Another plasmin inhibitor is macroglobulin.
There are also artificial plasmin inhibitors. These active ingredients include epsilon aminocarboxylic acids and epsilon amine caproic acids. In addition, para-aminomethylbenzoic acid (PAMBA) and tranexamic acid are each also an artificial plasmin inhibitor. Some of these active ingredients are used as antifibrinolytics for increased fibrinolysis.
Illnesses & ailments
As mentioned, hemostasis and fibrinolysis are in balance. Finely coordinated processes regulate activation and inhibition of thrombus formation and thrombus breakdown. Any disturbance of this balance can lead to serious illness.
For example, if there is increased blood coagulation without sufficient fibrinolysis, thrombosis can develop. Detached blood clots can migrate to the lungs, brain or heart and trigger embolisms, strokes or infarctions there.
There are many reasons for an increased tendency to thrombosis. In addition to increased blood coagulation due to underlying diseases and genetic predispositions, disorders in fibrinolysis are often responsible. It turned out that a disturbed fibrinolysis is the cause of a thrombosis or embolism with a share of 20 percent.
Plasminogen deficiency, tPA deficiency, low activity of tPA and protein C deficiency are discussed for the lower activity of fibrinolysis (hypofibrinolysis). Protein-C inactivates the coagulation factors Va and VIIIa through their degradation and induces the dissolution of the thrombi.
Hypofibrinolysis is often treated by administering plasminogen activators to drugs. In addition to hypofibrinolysis, there is also the clinical picture of hyperfibrinolysis. Here there is an increased breakdown of fibrin.
The result is an increased tendency to bleed. During hyperfibrinolysis, an increased spontaneous formation of plasminogen is often found. The effect is reinforced by the fibrin breakdown products, because they also inhibit the cross-linking of the fibrin molecules.
Another cause of the increased fibrinolysis can also be the inhibition of alpha-2-antiplasmin, the enzyme which deactivates the fibrin-degrading plasmin. If the deactivation is omitted, the breakdown of fibrin is no longer stopped. Hyperfibrinolysis is usually treated by administering artificial plasmin inhibitors.












.jpg)




.jpg)


