A Foot ulcer or Leg ulcer (Ulcus cruris) is a chronic skin damage on the lower leg, ankle or foot, which is usually due to disorders of the arterial or venous blood system. With age, the risk of foot or leg ulcers increases significantly.
What is a foot ulcer and leg ulcer?
.jpg)
© kayasit - stock.adobe.com
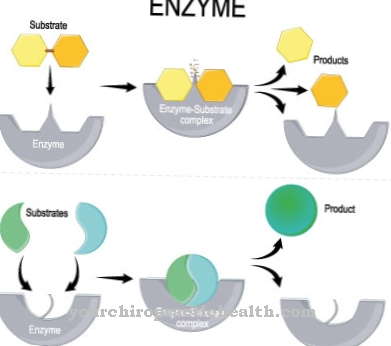
Chronic skin defects on the lower leg and foot that extend at least into the dermis are referred to as foot ulcers or leg ulcers (ulcus cruris). In the majority of cases (around 85%), a leg ulcer is caused by the venous leg (venous leg ulcer), that is, due to impairment of the venous blood circulation such as varices (varicose veins).
A venous leg ulcer occurs primarily on the inner ankle and medial lower leg and can extend to the fascia (covering of the connective tissue) or the bone below. In rarer cases, foot or leg ulcers are caused by insufficiency of the arterial blood circulation (ulcus cruris arteriosum) as a result of narrowed leg arteries (PAD, smoker's leg).
An ulcus cruris arteriosum is mostly localized on pressure points such as heels or toes and manifests itself as cool, pale skin with possibly livid (bluish) discoloration.
causes
The majority of foot or leg ulcers are caused by chronic venous insufficiency (CVI), which is often due to so-called varices (varicose veins or widening of the veins). Varices, the formation of which is usually a genetic predisposition (predisposition), impair the closing function of the venous valves.
This leads to edema (water retention) and then the connective tissue hardens (sclerosis). Edema and sclerosis cause an undersupply of the surrounding tissue structures with oxygen and nutrients, especially in the area of the ankles and the medial lower leg (front), which can lead to foot or leg ulcers. In addition to varices, thrombosis (blood clots) in the deeper leg veins can cause chronic venous insufficiency and thus foot or leg ulcers.
The rarer arterial foot and leg ulcers can be caused by arteriosclerosis (calcification of the arteries). Diabetes mellitus, nicotine consumption, hypertension (high blood pressure) and hyperlipidemia (high blood lipid level) are risk factors for arteriosclerosis in the legs and accordingly for foot and leg ulcers.
Symptoms, ailments & signs
The leg ulcer is characterized by ulcers on the legs and feet. It can be venous as well as arterial. The symptoms of both forms of the disease are slightly different. In the case of venous leg ulcers, the blood can no longer be adequately transported to the heart due to a weak vein.
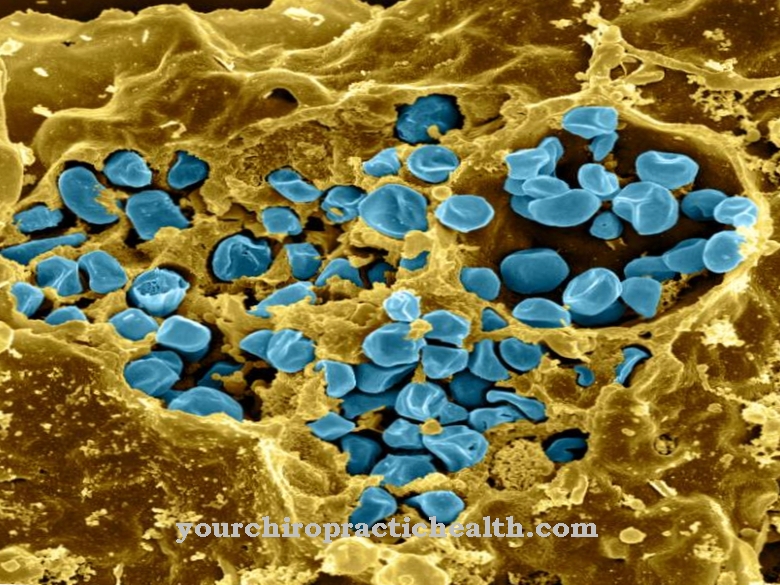
Swelling (edema) occurs in the area of the legs. The lack of nutrients in the tissue there results in wounds that are difficult to heal and that are constantly oozing. The escaping liquid softens the tissue at the wound edges and is often contaminated with bacteria if not handled properly. The degradation processes caused by bacteria lead to inflammation and foul-smelling degradation products.
Starting from the ankles, a venous leg ulcer often winds around the legs with enlargement and thus takes on the shape of a galosh. Pain rarely occurs. However, the venous leg ulcer is characterized by a constant feeling of tension in the affected limbs. An arterial ulcer is mainly found in the area of the feet. In contrast to the venous leg ulcer, however, severe pain occurs here.
This is especially true when raising your feet or when moving. In addition, arterial leg ulcers can cause necrosis of the undersupplied tissue when they turn black. Both forms of leg ulcer require a very long treatment time. However, the chances of recovery are better with a venous leg ulcer than with the arterial form.
Diagnosis & course
Foot and leg ulcers can usually be diagnosed based on the characteristic skin changes in the affected areas. A special ultrasound examination (Doppler sonography) enables statements to be made about possible arterial and venous circulatory disorders, while thromboses are made visible in the context of a phlebography (X-ray with contrast agent).
Determining the blood sugar levels provides information about the presence of diabetes mellitus. If there are indications of an infection, the pathogen is detected by means of a smear. A biopsy reveals a spinalioma (squamous cell carcinoma) as the cause of a leg ulcer.
As a rule, leg ulcers, especially venous leg ulcers, show a good course and heal within a few months, depending on the general health of the person concerned.
Complications
With this disease there are considerable complications and complaints that can lead to disorders and restrictions on the feet and legs. In most cases, this can result in a very unpleasant odor on the affected areas and wounds that are too wet. There is also severe pain in the legs and feet, which leads to restricted mobility.
The pain can also occur in the form of resting pain and thus lead to sleep problems and general irritability of the patient. As the process progresses, the skin turns bluish and the feet become cold because the blood circulation can no longer be properly regulated. The patient's quality of life is significantly reduced by the disease.
Due to the constant pain and restricted mobility, the patients often suffer from depression and other mental disorders. The treatment is always causal and depends on the underlying disease that is responsible for the ulcer. Often there is a positive course of the disease without complications, but in some cases surgical interventions are necessary to resolve the symptoms. The patient's life expectancy remains unchanged.
When should you go to the doctor?
If there is any unusual swelling on the feet or legs, a doctor should be consulted. Clarification of the cause is necessary if locomotion is impaired or the body is tilted. If the existing footwear no longer fits or if gait insecurity occurs, there is cause for concern. A doctor should be presented with a feeling of pressure in the leg, impaired sensation or numbness on the skin.
Changes in the appearance of the skin and discoloration of the skin are considered signs of existing diseases. These must be examined and treated. If everyday tasks can no longer be performed and participation in sporting activities or the usual leisure planning is no longer possible, a medical check-up is necessary.
If the symptoms increase or if the ulcer continues to spread, a doctor should be consulted immediately. If circulatory disorders occur, the extremities become very cold or warm and the frequency of movements is restricted. A doctor should be consulted.
In the case of emotional problems, behavioral problems or an increase in weight, it is also advisable to discuss the observations with a doctor. Changes in the odor and open wounds on feet and legs must be examined and treated. If pain in the legs persists for several days, it is necessary to clarify the symptoms.
Doctors & therapists in your area
Treatment & Therapy
In the case of foot and leg ulcers, the therapeutic measures are primarily aimed at eliminating the underlying causes. Venous leg ulcers are treated by improving the disturbed blood return by using compression bandages.
In addition, a leg ulcer should be treated with fibrinolytic ointments and / or antiseptic wound compresses for wound cleaning. As part of a surgical procedure, the varices tapering towards the leg ulcer can be removed or obliterated (sclerotherapy) to improve blood flow. In the case of poorly healing venous foot and leg ulcers, drugs that promote cell growth are often used to accelerate wound healing.
In addition, electrotherapy with direct current and laser therapy with a bundled, electromagnetic beam of light promote cell growth and wound healing. If there is a bacterial infection in addition to the leg ulcer, antibiosis (antibiotic) therapy is usually recommended. In many cases a leg ulcer is accompanied by allergic contact eczema, which is treated locally with cortisone.
In addition, fly larvae that feed on the dead tissue can be used for bio-enzymatic wound cleaning. In addition, a bypass operation, during which the disturbed section of the blood vessel is bridged with the help of a natural or artificial vein or artery piece to remove the circulatory disorder, can be indicated in the case of a leg ulcer.
prevention
Foot and leg ulcers can be prevented by taking measures to stimulate blood circulation, such as regular exercise, especially of the feet and legs while working on the computer. In addition, renouncing or restricting nicotine consumption reduces the risk of vascular diseases. Any excess weight should also be reduced to prevent foot and leg ulcers.
Aftercare
In the case of leg ulcers, the follow-up measures are usually very limited. First, the ulcer must be completely removed so that it cannot spread any further. For this reason, a very early diagnosis is necessary to prevent further complications and, in the worst case, the occurrence of a tumor.
Therefore, the leg ulcer should be examined and treated by a doctor as soon as the first symptoms appear. In most cases, those affected with leg ulcers are dependent on surgery. Bed rest should be kept for several days after the procedure so as not to put unnecessary strain on the body. Above all, the legs and feet should be rested and not unnecessarily strained so as not to slow down the healing of the wound.
Wearing compression stockings can also alleviate the symptoms of leg ulcers. These should be worn regularly. In some cases, physical therapy measures are also required to restore the person's movement. Some exercises can also be performed by the patient himself at home. Whether the leg ulcer leads to a reduced life expectancy cannot be universally predicted.
You can do that yourself
Foot ulcers and leg ulcers must be treated properly by the doctor to prevent progression and complications. As a support, compresses with diluted marigold extract or arnica tincture can promote healing, in some cases treatment with medicinal honey can be successful.
During the healing phase, the affected leg should be raised as often as possible. However, exercise is extremely important in order to stimulate blood flow. This applies both during treatment and after the ulcer has healed to prevent relapse.
In particular, long periods of sitting and standing inhibit the unimpeded flow of blood in the legs, so regular breaks in movement and changes of position are advisable. Great emphasis should be placed on comfortable, non-restrictive footwear, phases of rest can be used to raise the legs. Hot tub baths and long sunbathing are not beneficial for the health of the leg veins, whereas cold showers stimulate the blood circulation.
Continuing the compression therapy prescribed by the doctor can significantly reduce the risk of relapse - it is also important to eliminate risk factors such as obesity and smoking. Improper foot care often leads to small injuries, from which a leg ulcer develops. Diabetics in particular should therefore prefer professional medical foot care and also ensure that their blood sugar levels are well adjusted. Medical care for small wounds can often prevent ulcers from developing.

.jpg)














.jpg)