The term Gastroparesis refers to a disorder of the motility of the stomach. The paralysis of the stomach causes pain, nausea or vomiting.
What is gastroparesis?

© bilderzwerg - stock.adobe.com
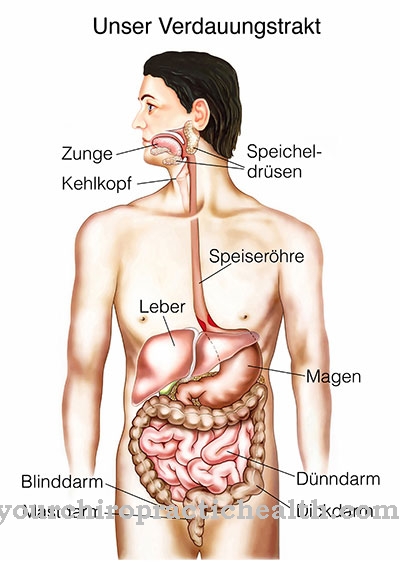
With gastroparesis, gastric motility is limited. Motility disorders are disorders of the healthy movement patterns of the digestive organs. The muscles of the stomach largely consist of smooth muscles. With gastroparesis, there is a decreased motility. This means that the smooth muscles of the stomach no longer move and contract sufficiently.
Thus, the mobility of the stomach is reduced or even completely eliminated. As a result of this gastric paralysis, the emptying of the stomach is disturbed. The term is also synonymous with the term gastroparesis Gastric atony utilized. Atony means something like slackness, whereas paresis is incomplete paralysis. The paralysis of the stomach can have various causes.
For example, damage to the enteric nervous system can be responsible for the paralysis. Stomach paralysis often has a significant impact on the quality of life of those affected and can also lead to serious complications in an emergency. Various drugs are used to treat gastroparesis. Surgery or artificial nutrition are also possible therapy options.
causes
The most common cause of gastroparesis is diabetic neuropathy. Diabetic neuropathy is damage to the nerves caused by the permanently high blood sugar levels. It is one of the most common secondary diseases of diabetes. Every third patient with diabetes mellitus suffers from sensitive disorders of the peripheral nerves.
However, the vegetative nervous system is also often affected. It controls the activity of many organs and, among other things, the activity of the stomach. When the nerves within the muscles of the stomach are disturbed or even destroyed, motility is severely impaired. Damage to the enteric and autonomic nervous systems is also known as autonomic neuropathy.
The nervous system can also be damaged by autoimmune diseases. Damage can also be inflammatory or hormonal. Hereditary diseases such as hereditary sensorimotor neuropathy type IV can also result in gastroparesis. The nerves are more rarely damaged by alcohol or nicotine abuse or by surgery. Most iatrogenic gastroparesis is caused by a vagotomy.
Vagotomy is a procedure used to treat stomach and duodenal ulcers. During the surgical procedure, the branches of the tenth cranial nerve, the vagus nerve, are cut. This should reduce the production of acidic gastric secretion. Because of the very effective proton pump inhibitors that are now available on the market, vagotomy is no longer often performed.
Gastroparesis can also accompany a migraine attack. The exact pathomechanisms are still unknown here. But gastroparesis does not only occur after nerve damage. The smooth muscles of the stomach can also be responsible for the paralysis. There are many different muscle diseases that can cause stomach paralysis. This includes, for example, progressive muscular dystrophy. In this disease, muscle weakness and muscle wasting are in the foreground.
Symptoms, ailments & signs
The symptoms of gastric paralysis are caused by impaired emptying. Patients feel full after eating. You suffer from nausea and vomit undigested food. Patients have little appetite and consequently lose weight.
Reflux esophagitis is a common complication of gastroparesis. In gastroparesis, the gastric sphincter is also paralyzed. As a result, the stomach and esophagus are not sufficiently separated from each other. Food and stomach acid go back into the esophagus. In particular, at night, after meals or when bending down and lifting loads, patients break down gastric juice.
The stomach acid irritates the mucous membranes of the esophagus, causing burning pain in the chest area. The irritation can also cause inflammation of the larynx (gastric laryngitis). Another typical symptom of reflux esophagitis is chronic cough. This is often wrongly interpreted as asthma.
diagnosis
If reflux esophagitis is suspected, gastroscopy is performed. During the examination, the doctor inserts a special endoscope, known as a gastroscope, into the stomach through the esophagus. The endoscope is usually equipped with a camera so that the doctor can assess the condition of the organs directly on a monitor. Gastroparesis is established by determining the gastric emptying time. Octanoic acid and sodium acetate are used for this.
Complications
In the context of gastroparesis, the disturbed emptying of the stomach can lead to various complications. At first, patients feel a strong feeling of fullness, which is often associated with nausea and vomiting. This can lead to severe weight loss.
If the gastric paralysis persists over a longer period of time, further gastrointestinal complaints can develop, which intensify the original clinical picture of gastroparesis. A typical complication is reflux esophagitis, in which food components and stomach acid return to the esophagus. This leads to belching especially after meals or when lifting loads.
If the reflux disease is not treated promptly, inflammation can develop in the throat. In the worst case, reflux esophagitis can develop into pneumonia. Larynx infections or chronic coughs develop more frequently. During the drug treatment of gastroparesis, allergies and intolerances can occur.
The prescribed prokinetics and antiemetics can also lead to cardiac side effects (cardiac arrhythmias) as well as sweating and physical restlessness. Treatment with an endoscope can rarely result in injuries to the gastric mucous membranes. If parenteral nutrition has to be initiated, further complications can arise.
When should you go to the doctor?
If you experience pain in the epigastric region, recurring nausea or vomiting, a doctor should be consulted. If the pain intensifies or spreads, a doctor is needed. Consultation with a doctor is required before taking any pain medication. There may be other complications or symptoms that need to be prevented. If the person concerned suffers from bloating, loss of appetite, or if food intake is reduced, a doctor should be consulted.
If you experience severe weight loss or eating disorders, a doctor is also needed. If undigested food can be detected during bowel movements, this observation should be discussed with a doctor. If symptoms of the larynx develop and a change in vocalization can be perceived, this is considered unusual and should be examined medically. If coughing persists or breathing noises, a doctor should be consulted.
If there is any inner restlessness, a feeling of illness or psychological problems arise, a doctor should be asked for advice. If the person concerned suffers from continuous unpleasant burping shortly after eating, this should be investigated. If food residues are regularly transported back into the esophagus when lifting or bending over, a doctor should be consulted.
Doctors & therapists in your area
Treatment & Therapy
In the case of a newly diagnosed or weakly developed gastroparesis, nutritional advice is given first. The symptoms can be alleviated, especially in the early stages, by a good supply of fluids and vital substances. In addition, patients should prefer low-fat foods with little fiber. The food should be divided into several small meals a day.
Prokinetics and antiemetics are used for drug treatment. Prokinetics stimulate the activity of the stomach and intestinal muscles and thus cause the stomach to empty more quickly. Antiemetics work in the vomiting center and suppress vomiting and nausea. However, they do not affect gastric motility. Artificial nutrition may be necessary in severe or long-lasting paresis.
Liquid nutrients are fed into the stomach or small intestine through a tube. Nutrients may also be administered parenterally. To do this, a nutrient solution is injected into the patient's vein. Parenteral nutrition is chosen when enteral nutrition is not well tolerated. Even if sufficient energy cannot be supplied through enteral nutrition, parenteral nutrition is used.
Outlook & forecast
It plays a major role in the prognosis whether the gastroparesis is caused by another disease that is curable or can be easily controlled, or whether the cause is irreversible. If the cause cannot be treated, gastroparesis persists in the majority of cases. This danger also exists if treatment is theoretically possible, but the patient refuses or does not follow therapy.In either case, it is possible that gastroparesis will worsen.
Gastroparesis can occur as a result of diabetes and other diseases. In this case, if the patient changes their lifestyle and overall diabetes is well under control, the prognosis improves. Patients who smoke and give up this addiction also increase their chances of symptom improvement.
Diabetic gastroparesis does not seem to affect the death rate (Chang, Rayner, Jones & Horowitz, 2013). Overall, however, the treatment of diabetic gastroparesis is considered complicated. For this and other forms of gastroparesis, doctors often recommend a special diet plan that is geared towards frequent and small meals. A nutritionist can help put the recommendations into practice.
prevention
The most common cause of gastroparesis is diabetic neuropathy. This can be prevented by a well-adjusted blood sugar in diabetics.
Aftercare
In most cases, there are no special follow-up options available to those affected by gastroparesis. The focus is on medical treatment of the disease in order to prevent further complications and complaints. As a rule, self-healing cannot occur, so treatment by a doctor is essential.
In general, a healthy lifestyle with a balanced diet has a very positive effect on the further course of gastroparesis and can significantly accelerate healing. The person affected should avoid fiber as much as possible and eat healthily. It is also necessary to take medication.
The affected person should always ensure that they are taken regularly, taking into account possible interactions with other drugs. Parents should ensure that the medication is taken regularly, especially with children. In some cases, regular gastric examinations are useful in order to identify and treat damage to the stomach that has already been shown.
It cannot be universally predicted whether the life expectancy of the person affected will be reduced by gastroparesis. Contact with other affected persons can also be useful, as this leads to an exchange of information that can make everyday life much easier.
You can do that yourself
In the case of gastroparesis, a doctor should definitely be consulted. Medical therapy can be supported with the help of some self-help measures and home remedies.
First of all, it is necessary to adapt the diet to the disease. Foods with a high fat content should be avoided at all costs, as these foods slow down digestive activity. Low-fat alternatives such as lean meat, low-fat milk, cottage cheese, egg whites, and yogurt are better.
In general, a balanced, low-fiber diet with lots of fish, tofu, white bread and canned vegetables is recommended. These foods can be pureed and consumed to speed up digestion. If you don't want to do without solid food, you should chew every bite well and drink plenty of water. Protein shakes, clear soups and broths as well as drinks rich in electrolytes have also proven their worth.
A tried and tested home remedy is ginger tea. The healthy medicinal root promotes the formation of gastric juice and supports intestinal activity. Peppermint tea is just as effective, relaxing the stomach muscles and promoting the production of bile.
In addition to these dietary measures, sufferers should record the triggers for complaints in a diary. In this way, a suitable nutrition plan can be put together with a nutritionist.

.jpg)


.jpg)