Of the Corpus luteum is formed from the follicle immediately after ovulation and consists of the egg cell and luteinized theca and granulosa cells. These cells are responsible for the cycle-appropriate production of progesterone and estrogen. If the corpus luteum is deficient, the cells produce too few hormones, which can make pregnancy difficult or lead to early abortion.
What is the corpus luteum?
The female cycle is controlled by hormones. The egg cell is released from the female ovary by certain hormones, for example, and migrates to the fallopian tube. The fallopian tube picks up the detached egg cell. This movement corresponds to ovulation, i.e. ovulation. Ovulation occurs around the middle of the woman's menstrual cycle and is often noticeable as a pulling pain in the lower abdomen.
This also occurs under hormonal control after ovulation Corpus luteum. This substance corresponds to the corpus luteum, which arises from the follicle. This is a hormone-producing cluster of cells that is either the corpus luteum menstruationis or the corpus luteum graviditatis. The first form arises from unfertilized egg cells. The second form refers to fertilized follicles. The influence of the luteinizing hormone (LH) is crucial for the development of the corpus luteum. Once it is formed, the corpus luteum controls the female cycle through internal hormone production.
Anatomy & structure
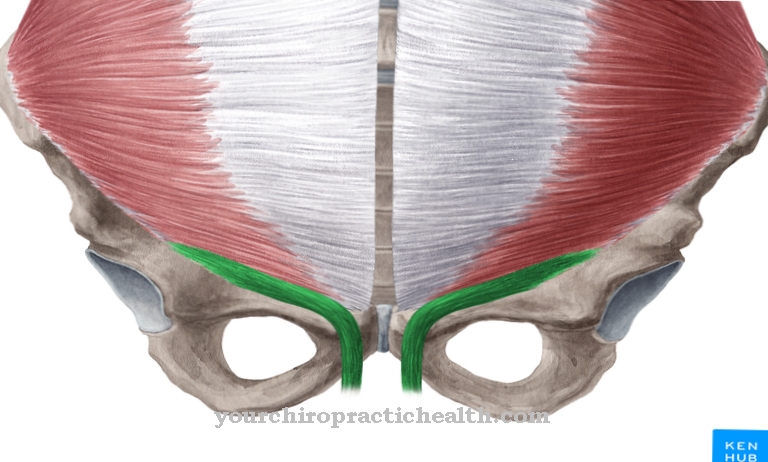
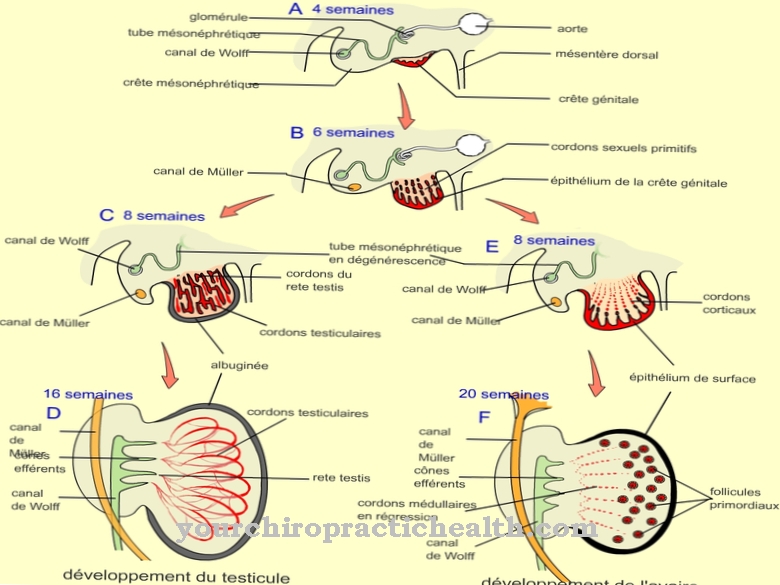
The corpus luteum arises from the follicle after ovulation. The female egg changes its shape immediately after ovulation. The basement membrane of the follicle dissolves. Under the influence of LH, the contained theca and granulosa cells are transformed into so-called granulosalutein cells and thekalutein cells. This process corresponds to luteinization.
Shortly before this process, a preliminary stage of the corpus luteum, the corpus haemorrhagicum, forms. This preliminary stage arises from the spontaneous hemorrhage into empty ovarian follicles. The blood is resumed shortly after the bleeding and the luteinization of the granulosa and theca cells begins. As soon as the luteinization is complete, the corpus haemorrhagicum has changed to the corpus luteum. If the egg cell is not fertilized in a menstrual cycle, the corpus luteum recedes.
Around nine days after ovulation, the corpus luteum reaches its maximum size and from then on continuously decreases in size due to connective tissue degeneration. If, on the other hand, the egg cell is fertilized, the hormones secreted from now on cause the corpus luteum to rapidly increase in size. The cells involved in the tissue begin to proliferate.
Function & tasks
The corpus luteum is used to produce hormones. The granulosalutein cells contained are hormone-producing cells that can produce progesterone. The gynecologist also knows progesterone as a corpus luteum hormone. After ovulation, progesterone is produced in daily amounts of around 20 to 50 milligrams.
The progesterone level in the blood increases bit by bit. Within a few days, the blood level reaches 50 to 100 times this value and is around 10 ng per milliliter. The thekalutein cells in the corpus luteum are also responsible for the production of hormones. Instead of progesterone, these cells produce the female estrogens. The high level of progesterone keeps the gonadotropin level at a low level during the luteal phase. This principle follows a negative feedback principle to the pituitary gland and prevents further egg cells from maturing during this time.
If the matured egg cell is not fertilized, the theca and granulosa cells in the corpus luteum produce less estrogen and progesterone. The resulting drop in blood level initiates the breakdown of the endometrium. Menstruation begins. If the egg cell does not remain unfertilized, the human chorionic gonadotropin (HCG) prevents gel body degeneration. Nothing stands in the way of the growth of the corpus luteum. The corpus luteum produces pregnancy-maintaining hormones after fertilization.
In about the ninth week of pregnancy, the cells produce estrogens and progesterone. From the tenth week onwards, a luteoplacental shift occurs. The hormone production no longer takes place in the corpus luteum, but in the fetoplacental unit or placenta.
You can find your medication here
➔ Medicines for menstrual crampsDiseases
The corpus luteum can develop cancer. The theca and granulosa cells, from which benign and malignant tumors can originate, are susceptible to this. Tumors based on theca and granulosa cells are hormone-producing tumors that disturb the hormone level through their profileration.
Hormone-related symptoms such as unscheduled bleeding can be the first signs. Almost every age group can be affected by the tumors. Insufficiencies of the corpus luteum are even more common than tumors of the gel body. Like all other insufficiencies, those of the corpus luteum are also expressed in a general functional weakness of the anatomical structure. The cells involved produce less progesterone and estrogen in luteal insufficiency. The plasma concentration of the corpus luteum hormones falls. As a consequence, the luteal phase of the cycle is shortened.
Under these conditions, the endometrium cannot transform itself properly. This phenomenon makes pregnancy difficult in many cases. Some of the women affected find it difficult to conceive at all. Others become pregnant but cannot maintain the pregnancy.
The insufficiency of the corpus luteum is the most common cause of miscarriages in the sense of an early abortion. Many of the patients experience several early abortions in their lives. In the meantime, hormonal substitution has become established as a treatment for luteal insufficiency. Since progesterone is particularly relevant as a pregnancy hormone, the affected women are intravenously administered the luteal hormone including its derivatives.



















.jpg)



