As Hepatoblastoma is a rare malignant (malignant) embryonic tumor on the liver that mainly affects infants and young children. If the tumor is diagnosed early enough before it metastasizes, surgical removal of the tumor offers a good chance of survival.
What is hepatoblastoma?

© matis75– stock.adobe.com
The hepatoblastoma is an embryonic tumor on the liver, i.e. it arises on liver cells that are not yet fully differentiated. It mostly affects infants and young children with a maximum frequency between the ages of 6 months and 3 years.
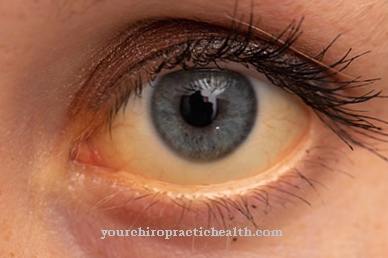
Children over the age of 15 will only develop hepatoblastoma in exceptional cases. In the beginning there is hardly any pain, so that the tumor - especially since it occurs rarely - is usually only noticed during routine examinations. The hepatoblastoma is usually palpable and in some cases there may be visible abnormal liver function due to yellowing of the skin.
The embryonic tumor is subject to different physiological conditions and requires different therapies than a liver tumor on fully differentiated liver cells (hepatocellular carcinoma) and must therefore be distinguished from it.
causes
The hepatoblastoma is causally associated with various genetic defects, which also affect the rare Beckwith-Wiedemann syndrome (one-sided, asymmetrical giant stature) or other half-sided growth problems.
Hepatoblastomas are also associated with familial, autosomal dominant inherited adenomatous polyposis (development of a large number of polyps in the large intestine) and with extremely premature births. Japanese studies have shown a significant statistical correlation between the incidence of hepatoblastoma and birth weights of less than 1,000 g in premature births.
The extent to which this is a coincidental or causal relationship has not yet been conclusively clarified. There is also an (as yet) unsettled connection to Li-Fraumeni syndrome, which is caused by a mutation in a tumor suppressor gene in the germline and can lead to multiple tumors at an early age.
Symptoms, ailments & signs
Initially, a hepatoblastoma is often not noticeable symptomatically. Only a painless swelling of the abdomen in the child is occasionally observed. The disease usually begins before the end of the second year of life. In rare cases, the onset of the disease later or earlier is possible.
Boys are more often affected than girls. After a longer symptom-free period, the affected children suffer from nausea, vomiting and weight loss. Before this, in rare cases, abdominal pain and jaundice can occur if the tumor leads to an obstruction of the biliary tract at an early stage.
Overall, the disease is characterized by an increasing general weakness. Developmental delays occur, but they only become noticeable after a long period of illness. In boys it can come to an early puberty (pubertas praecox). Further symptoms only appear when metastases form. These depend on which organs are affected by the metastases.
The lungs are most commonly affected. This often leads to breathing difficulties, coughing fits and sometimes blood spitting. In rare cases, metastases to the bones, bone marrow, and brain occur. This leads to bone pain, frequent bone fractures, severe restrictions on movement, seizures, tendency to bleed, anemia and general fatigue. With timely treatment and complete removal of the tumor, there is a good chance of a complete cure.
Diagnosis & course
If hepatoblastoma is suspected for the first time, several diagnostic methods are available that can complement each other. First of all, a non-specific laboratory test is recommended, in which, in addition to platelets and ferritin, the LDH concentration (lactate dehydrogenase) and liver enzyme values are determined.
An increased LDH concentration provides an indication of cell or organ damage in the body. A specific laboratory test should provide information on whether the tumor marker alpha-fetoprotein (AFP) is significantly increased, because this value is increased in 80% - 90% of cases and, conversely, a hepatoblastoma is definitely present with corresponding AFP values.
Diagnostic imaging methods such as abdominal ultrasound, chest X-ray, thorax CT or upper abdominal CT, each with contrast media, are available for further clarification. Histopathological examinations should also be performed to confirm a positive diagnosis. The course of the disease, if left untreated, leads to liver failure and the formation of metastases, predominantly in the lungs, so that a fatal course is predicted.
Complications
Because hepatoblastoma is a tumor, it has the usual symptoms and complications of cancer. In the worst case, this can lead to the patient's death if the tumor spreads to other regions of the body and causes damage there. If the hepatoblastoma is diagnosed and removed early, life expectancy is usually not reduced.
The hepatoblastoma primarily leads to severe abdominal pain and jaundice. The stomach swells up and appears bloated. Those affected also suffer from vomiting and nausea. It is not uncommon for the symptoms to also lead to weight loss and deficiency symptoms. The symptoms often lead to psychological moods and irritability in the patient.
If the hepatoblastoma is not treated, metastases usually develop in the lungs and liver, causing both organs to fail. This leads to the death of the patient. With an early diagnosis, the tumor can be removed. The further course of the disease depends on the region and the extent of the tumor. In some cases, a transplant is necessary if the internal organs have been damaged.
When should you go to the doctor?
Parents who notice signs of jaundice in their child should contact the pediatrician. If the symptoms persist for more than two to three days, a serious illness is suspected. A specialist must clarify the symptoms and, if necessary, initiate treatment.
A diagnosed hepatoblastoma is a serious illness. Parents should consult the responsible doctor regularly and inform the doctor about unusual symptoms. If metastasis is suspected, the doctor will perform a comprehensive ultrasound scan and refer the parents to a specialist for further treatment.
The tumor may initially spread without being noticed, but sometimes it causes symptoms. For example, if the child feels severe pain, is particularly irritable or has difficulty breathing, an immediate doctor's visit is indicated.
Nausea, vomiting or spitting blood should also be clarified, as these symptoms indicate that the tumor has metastasized into the lungs. A hepatoblastoma usually needs to be removed surgically or with chemotherapy or radiation therapy. After treatment has been completed, the parents must continue to watch out for abnormalities and have the child regularly examined by a doctor.
Doctors & therapists in your area
Treatment & Therapy
The aim of every therapy is to remove the tumor completely and to observe the further postoperative course of the disease in initially narrow time intervals of 6 weeks. If the hepatoblastoma is classified as inoperable, prior chemotherapy containing cisplatin may be necessary.
Radiation therapy has hardly any effect on this disease and is therefore out of the question. After chemotherapy is complete, the tumor is surgically removed, which is only possible if it is restricted to specific areas of the liver. If the hepatoblastoma is not (yet) operable after the first chemotherapy, further chemotherapy may well be worthwhile in order to take another chance to let the tumor develop back into an operable state.
During the total resection of the tumor, care is taken to ensure that no residual tissue is left that could quickly develop into a relapse. Postoperatively, there is another chemotherapy, which should contain a combination of cytostatics, if possible, since hepatoblastomas can develop resistance to cisplatin as the only active ingredient.
In the case of children with inoperable tumors who also do not respond to preoperative chemotherapy, the alternative is to close the supply and discharge vessels that supply the tumors in order to interrupt the supply of the tumors as far as possible.
Otherwise, the last treatment option is a liver transplant. In follow-up care after a total resection of the tumor, the development of the AFP tumor marker is crucial. A further increase indicates the development of a new tumor one to two months before a relapse that can be diagnosed with imaging methods.
Outlook & forecast
The prognosis for hepatoblastoma depends on the treatment. She is good with therapy. Without treatment, the disease always leads to death. It is a cancer of the liver that has four stages. In the course of the disease, metastases often develop in the lungs. The brain, bones and bone marrow are less commonly affected.
If the therapy does not start until after the first metastases have appeared, attempts can only be made to increase the life expectancy of the children and to maintain or restore the quality of life. Whether a complete or at least long-term cure can be achieved under these circumstances depends on the individual case. As a rule, however, complete healing is no longer possible when metastases occur.
Nevertheless, the chances of recovery from hepatoblastoma are very good if the tumor is completely removed before metastases develop. No residues must remain in the body. However, this can be done very well by performing cytostatic therapy before the operation.
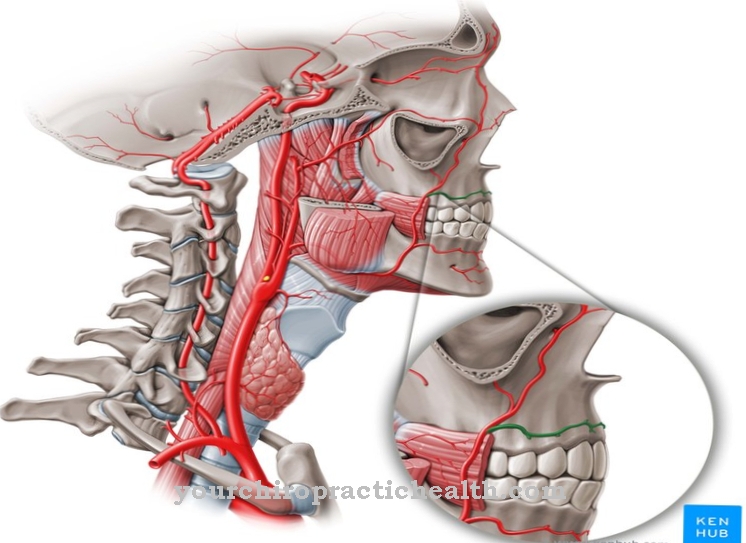
With this therapy, in which certain cytostatics are applied to the arteria hepatica, the certainty that the primary tumor can be localized and resected without residues increases. This increases the five-year chance of survival with a hepatoblastoma to about 80 percent. So eight out of ten children can be completely cured with a complete resection of the tumor.
prevention
A sensible prophylaxis to avoid a hepatoblastoma is not possible, since the development of the disease is very likely based on inherited genetic defects or genetic anomalies. Therefore, a family history is important. If specific cases of illness are known in the family, it is advisable to closely monitor the child and, if necessary, to regularly check the AFP tumor marker as a prophylactic.
Aftercare
In most cases of hepatoblastoma, there are very few follow-up options available to those affected. In the worst case, the disease can lead to the death of the person affected if it is recognized late. Therefore, early detection and subsequent treatment are the main focus of this disease. A doctor should be consulted at the first signs and symptoms so that there are no further complications.
The tumor is usually removed by surgery. After such an operation, the person concerned must definitely rest and take care of his body. Here you should refrain from exertion or other stressful or physical activities in order not to unnecessarily burden the body.
Often the patients are also dependent on the support and help of their own families, which can alleviate psychological moods or depression. Even after the hepatoblastoma has been removed, regular examinations of the internal organs by a doctor are often necessary. The taking of medication is often useful, whereby it is important to ensure the correct dosage with regular use.
You can do that yourself
A heptoblastoma is usually treated with chemotherapy or radiation therapy. Those affected can support the treatment through various measures.
Until the start of therapy, those affected have time to collect information and find a way to deal with the disease. Basically, body and mind must be prepared for the treatment. Heptoblastoma patients should exercise enough, take in enough nutrients, and drink a lot just before chemotherapy.
Many side effects can be alleviated by means of complementary medicine, such as bitter substances against loss of appetite and the homeopathic preparation Nux vomica against nausea and vomiting.
There are also many ways to support recovery during therapy. For example, moderate endurance sports are recommended - in the best case, regularly and outdoors - because exercise promotes oxygen supply and improves the cell environment. A healthy and balanced diet can also alleviate the debilitating effects of chemotherapy and help the body fight heptoblastoma.
The menu should primarily contain foods that are rich in trace elements and vitamins. In consultation with the doctor, targeted purification can also be carried out in order to deacidify the body and remove the nutrient medium from the cancer cells.



.jpg)
.jpg)


.jpg)