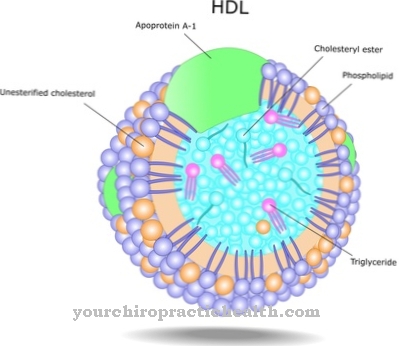
High density lipoproteins represent one of several classes of transport molecules that transport cholesterol esters and other lipophilic substances in the blood plasma.
HDLs take over the transport of excess cholesterol from the tissue to the liver. In contrast to the low-density lipoproteins, which are responsible for the opposite transport of cholesterol, HDLs are also referred to as "good" cholesterols, because they contain e.g. B. absorb excess cholesterol from the vessel walls and transport it away.
What are high density lipoproteins?
High Density Lipoproteins (HDL) are made up of around half of proteins and the other half of cholesterol esters, triglycerides and phospholipids.
They can be divided into four further subclasses. The proteins mainly consist of so-called amphiphilic apolipoproteins (ApoLp). As high-density lipoproteins, they form one of five classes. The other lipoprotein classes are Low Density (LDL), Very Low Density (VLDL), Intermediate Density Lipoproteins (IDL), Chylomicrons and Lipoprotein a (Lp (a)). Lipoproteins of all classes are ultimately transport molecules that transport water-insoluble lipophilic substances such as cholesterol esters in the blood plasma to or from target organs. Lipoproteins with a density of 1.063 to 1.210 g / l are included in the HDLs. The molecules only reach a size of 5 to 17 nanometers.
The structure and size of HDLs vary depending on the cholesterols, lipids and triglycerides that the HDL molecule transports. The class of HDL is considered beneficial from a physiological and medical point of view, because cholesterol and other substances are absorbed from certain tissues and transported to the liver, so that atherosclerotic plaques (calcifications) in blood vessels, which mainly consist of deposited cholesterol, can improve. In contrast, LDLs transport cholesterol from the liver to the target tissue, including the walls of the blood vessels. In principle, HDLs are therefore referred to as physiologically favorable and LDLs as physiologically unfavorable (“bad”).
Function, effect & tasks
Cholesterols are extremely important for the body's metabolism. They are a necessary component of all cell membranes, including the epithelia in the blood vessels.
In addition, cholesterols perform important functions in the brain. Low cholesterol is associated with decreased cognitive and other brain functions. However, tiny injuries and tears in the blood vessels can trigger an excessive repair process, so that deposits can form in the vessels, which can lead to an arteriosclerotic narrowing and a loss of elasticity in certain blood vessels. Because a high proportion of the plaques in the vessels consists of cholesterol, a high cholesterol level has been considered harmful to health for decades.
In this context, HDL plays a positive role as a transport molecule, as it transports excess cholesterol from the tissue to the liver, where it is further metabolized, i.e. broken down or recycled. In contrast, the main task and function of the LDL fraction of lipoproteins is to transport cholesterol from the liver to the target tissue. The return transport of excess cholesterol carried out by HDL is also called reverse cholesterol transport. A high HDL level in the blood serum is considered to reduce the risk of coronary heart disease. In addition, atherosclerotic plaques can even regress and HDLs are associated with antipoptotic and antithrombotic effects.
Education, occurrence, properties & optimal values
The concentration of cholesterol in the body cannot be measured directly, but only indirectly by determining the lipoproteins and triglycerides in the blood serum. Due to the central importance of cholesterol for a large number of metabolic processes, the body is able to regulate the concentration of the individual lipoprotein classes by means of synthesis processes largely independently of the food consumed.
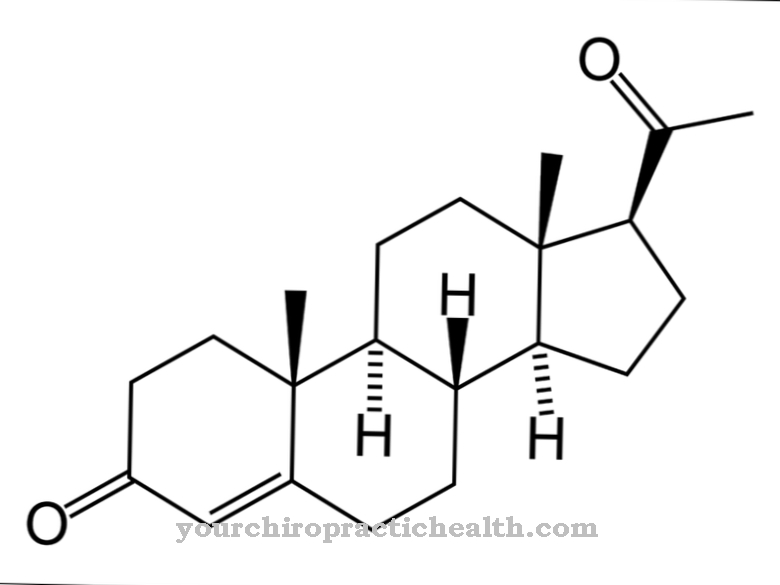
The starting point for biosynthesis is the so-called mevalonate pathway, via which DMAPP (dimethylallyl pyrophosphate) is produced. The DMAPP is mainly used in the liver, but also in the intestinal epithelium, to synthesize cholesterol in an 18-step process. Because the lipoprotein molecules are too large to cross the blood-brain barrier, the brain is able to produce the cholesterol it needs itself. The concentration of HDL in the blood serum seems to largely follow the genetic predisposition in connection with living conditions.
After decades of demonizing a high level of lipoproteins, the focus is more and more on the concentration of HDLs, on the assumption that HDLs transport excess cholesterol from the membranes of the blood vessels into the liver and thus counteract atherosclerotic vascular changes and all consequential damage. The ratio of LDL to HDL is also important. A quotient below three is considered positive, while quotients above 4 are considered unfavorable. Regardless of the ratio of LDL to HDL, a concentration of HDL below 40 ml / dl is considered unfavorable and a value above 60 is favorable.
Diseases & Disorders
A low HDL level in the blood serum of less than 40 ml / dl increases the risk of atherosclerotic changes in the blood vessels because the HDLs cannot adequately carry out their task of removing excess cholesterol.
This increases the risk of further consequential damage such as high blood pressure, heart attack and stroke. A one-sided decreased HDL synthesis can be caused by the rare Tangier disease. The genetic defect disrupts the protein apolipoprotein A1 (ApoA1), which is required to dissolve excess cholesterol from the tissue and attach it to the HDL. The disease is inherited as an autosomal recessive trait, so it affects men and women equally. Diseases such as type 2 diabetes also lead to a decrease in HDL levels. In addition to genetic predisposition, living conditions also influence the concentration of HDLs in blood serum.
A negative, i.e. lowering, influence on the HDL level has a sedentary lifestyle, smoking and being overweight. This means that if the concentration of HDL is too low, the normalization of body weight and an increase in physical activity have a positive, i.e. increasing, influence on the HDL concentration.