The hypertrophic cardiomyopathy is an inherited heart muscle disease. Medicine distinguishes between an obstructive and a non-obstructive form. Patients of the non-obstructive form are often long or even lifelong asymptomatic.
What is hypertrophic cardiomyopathy?

© HANK GREBE - stock.adobe.com
The group of cardiomyopathies summarizes diseases of the heart muscle. Cardiomyopathies are associated with mechanical or electrical functional limitations of the heart. However, they do not necessarily have to be associated with pathologically changed heart chambers. The hypertrophic cardiomyopathy will also be hypertrophic familial cardiomyopathy called. This condition is a congenital disease of the heart muscle.
In addition to an asymmetrical thickening of the left ventricle, the disease also has an expansion of the heart chambers. With a prevalence of 1: 500, familial hypertrophic cardiomyopathy is a comparatively common heart disease. Inheritance takes place in an autosomal dominant mode of inheritance. A distinction is made between two forms of heart disease: hypertrophic cardiomyopathy with dynamic obstruction and a form without dynamic obstruction.
According to the classification of the World Health Organization (WHO), all familial hypertrophic cardiomyopathies can be assigned to the genetically determined primary cardiomyopathies. The disease was described by Liouville and Hallopeau in the mid-19th century. It has been recognized as a clinical entity since it was described by Brock in the 20th century.
causes
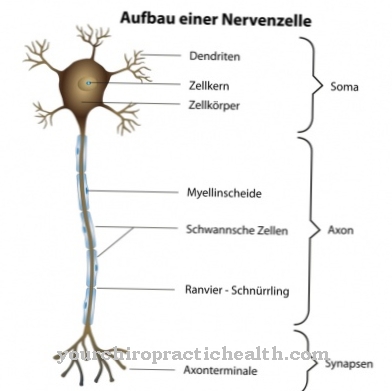
Hypertrophic cardiomyopathies are caused by genetic makeup. More than 200 genetic defects on ten different genes are known to be possible causes. The causative genes all code for the proteins in the cardiac sarcomere. In more than 50 percent of the cases, the genetic defect lies in the structure of the so-called beta-myosin heavy chain. The resulting structural changes in β-myosin and α-tropomyosin result from numerous point mutations in the structural proteins in the sarcomere, such as the myosin binding protein C or troponin T.
The hypertrophic cardiomyopathy is therefore also Sarcomere disease called. A large part of the point mutations affects the gene locus MYH7 on chromosome 14. Thus a branching disorder of hypertrophied heart muscle cells develops in the sarcomere. The parallel arrangement is missing due to increased lateral branching. The interstitium is remodeled with connective tissue. The phenotypic expression depends less on the individual mutation than that it is determined by environmental factors and modifier genes. Up to the age of 13 the disease is mostly silent.
Symptoms, ailments & signs
A quarter of patients suffer from a thickening of the heart muscle in the left ventricle, which is located in the outflow tract. This creates an obstruction during exercise, but also at rest. This results in an aortic stenosis with a high pressure load on the left ventricle. In about ten percent of patients, the obstruction is co-ventricular. The muscle thickening also causes muscle stiffening. The ventricle of the heart only fills to a limited extent during the relaxation phase and blood backs up in the veins of the lungs, causing shortness of breath.
This phenomenon is known as diastolic heart failure. The muscle stiffening increases in the course of the disease due to the forced pumping power. In the area of the narrowed outflow path, a suction is created, which is also known as the Venturi effect. Leakages in the sense of mitral regurgitation often occur. Cardiac arrhythmias occur during exercise, which can lead to brief loss of consciousness or even sudden cardiac death. Many young adult sudden deaths are caused by hypertrophic cardiomyopathy. Patients of the non-obstructive form are often asymptomatic. If there are symptoms, they are non-specific symptoms such as shortness of breath, dizziness or angina pectoris.
Diagnosis & course of disease
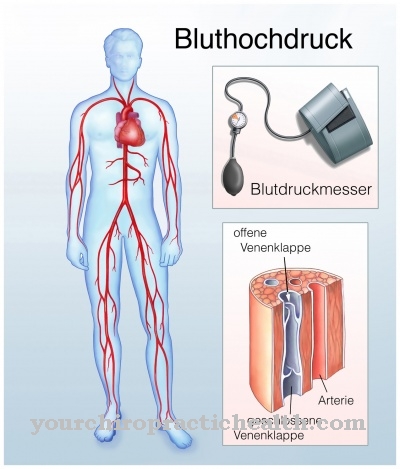
When diagnosing hypertrophic cardiomyopathy, reactive myocardial hypertrophy due to exercise (athlete's heart) or high blood pressure must be excluded. Diseases of the aortic valve should also be considered in the differential diagnosis. During the physical examination of the patient, a systolic appears which increases due to the exertion. This symptom can be observed in the context of the Valsalva maneuver.
Ideally, the ECG provides evidence of left ventricular hypertrophy by showing Q waves and a repolarization disorder. Echocardiography shows, in addition to septal hypertrophy, a shift in the mitral valve leaflet, which narrows the outflow tract. The resting gradient in the sense of a pressure jump between the left ventricle and the main artery is measured. Magnetic resonance tomography shows atypical forms of distribution and may show spotty scars in the myocardium.
In addition, the flow acceleration and possibly indications of previous septal embolizations can be displayed. A cardiac catheterization exam measures the pressure in the heart to determine if the heart is stiff. A molecular genetic examination confirms the diagnosis. Many asymptomatic patients have a rather low level of impairment and therefore a good prognosis. Forms with obstruction of the left ventricular outflow tract often develop into heart failure and therefore have a poorer prognosis.
Complications
Complications of hypertrophic cardiomyopathy arise from the possible symptoms and consequences. For example, cardiac arrhythmias can be dangerous. In this case, it is necessary to take medication to treat the irregular heartbeat. In addition, the risk of sudden cardiac death, death from heart failure and stroke is comparatively high, which makes hypertrophic cardiomyopathy the most complex and serious form of all cardiomyopathies.
Sudden cardiac death occurs in one percent of cases and is more likely to affect younger patients. Symptoms are usually mild, making it difficult to diagnose hypertrophic cardiomyopathy. It can also be observed that there is a higher risk for family members who have the same disease. Heart failure, the most common complication, plays a bigger role in older people.
Since the left outflow channels are increasingly stressed, they can narrow in the course of the disease. This can stiffen the heart muscle. A stiff ventricle results in atrial fibrillation, which affects 25 percent of patients. Endocarditis, an inflammation of the inner lining of the heart that spreads to the heart valves, can also occur as a secondary disease.
Overall, hypertrophic cardiomyopathy is an incurable disease, which in most cases runs without complications and has good treatment options. Life expectancy is not affected, this is only the case with severe disease.
When should you go to the doctor?
Any abnormalities in the heart rhythm should be examined by a doctor. If there is a feeling of pressure in the upper body, an internal heaviness or there are breathing problems, a doctor is required. Breathing disorders, shortness of breath or interruptions in breathing must be clarified immediately by a doctor. There is a threat of an undersupply of the organism, which can lead to multiple organ failure. Since hypertrophic cardiomyopathy can lead to sudden cardiac death without medical treatment, a visit to a doctor is recommended as soon as the first irregular heartbeat occurs.
If you experience palpitations, increased blood pressure, sleep disorders or inner restlessness, you should consult a doctor. In the event of chest pain, reduced performance or rapid exhaustion, examinations should be initiated to clarify the cause. If there is a disturbance of consciousness or if unconsciousness occurs, the person concerned needs an emergency doctor. A rescue service must be alerted and first aid measures must be initiated. In the event of dizziness, unsteady gait or impaired attention, a check-up visit with a doctor is recommended. A general feeling of illness or persistent malaise should be examined and treated. If the symptoms increase, a visit to the doctor is essential. If the physical irregularities are accompanied by emotional problems, a doctor is required.
Doctors & therapists in your area
Treatment & Therapy
Although hypertrophic cardiomyopathy has not yet been curable, it can now be treated symptomatically. The earlier the diagnosis is made, the better the prognosis. Drugs such as beta blockers to downregulate the left heart ventricle are available as conservative treatment measures. Antiarrhythmics reduce cardiac arrhythmias.
Patients are advised to avoid competitive sports and sports with sudden maximum stress. Catheter treatment of septal hypertrophy can be used as an interventional measure. This treatment is carried out by a transcoronary ablation of the septal hypertrophy or a percutaneous transluminal septal myocardial ablation. The anterior interventricular ramu is closed with a balloon through a cardiac catheter. When the gradient in the outflow tract drops, pure alcohol is chased through the balloon and triggers a circumscribed infarction in the obstruction area.
This reduces the obstruction. Another possible treatment modality is endocardial radiofrequency ablation of septal hypertrophy. Cardiac catheter-guided radio frequency ablation treats cardiac arrhythmias. Electrical energy is delivered through a cardiac catheter in the area of the obstruction to the right ventricle of the septum. Scarring reduces the gradient in the outflow tract of the left ventricle. An invasive treatment option is transaortic subvalvular myectomy.
This heart surgery removes muscle tissue from the outflow tract of the left ventricle through the aortic valve. Supportive measures are also available to patients with hypertrophic cardiomyopathy. For example, a defibrillator can be implanted against cardiac arrhythmias.
prevention
Hypertrophic cardiomyopathy cannot be prevented because the disease has a genetic cause.
Aftercare
The follow-up options for hypertrophic cardiomyopathy mainly focus on regular check-ups to ensure that the blood pressure is correctly adjusted. Depending on the symptoms, the doctor can expand this diagnosis or shorten the intervals between the examination appointments. In some cases, the patients have specialist doctors available who offer appropriate consultation hours.
The long-term follow-up should be stable, and the attending physician is responsible for monitoring it. It may be necessary to adjust the medication to avoid deterioration. In hereditary patients with an enlarged left ventricle, however, the risk of sudden cardiac death increases.
Those affected should avoid excessive physical exertion and should also be careful when exercising. If you overload yourself, the risk increases by leaps and bounds. If physical exertion is unavoidable, patients should not stop abruptly, but let it fade away gradually. The usual everyday activities are basically not a problem and do not lead to complaints.
Those affected do not have to do without swimming, traveling and light activities. If other surgical or dental interventions are necessary, the responsible physician must take the necessary precautions to protect the patient and minimize the risk.
You can do that yourself
In everyday life, the main thing is to avoid situations that are physically stressful. Depending on the usual physical resilience of those affected, this can include intensive sporting activity and competitive situations such as a football game or playing top-class sport. Heavy physical work should also be avoided. This is especially true if these are associated with strong pressing and pushing.
However, should a physically stressful situation arise, it is best not to end it abruptly, but rather to let it come to an end slowly. Most everyday activities, but also traveling or swimming, are entirely possible for those otherwise symptom-free. Sexual activities in a normal framework are unproblematic with normal everyday stress.
In order to prevent the development of further heart diseases, those affected should refrain from smoking. It is also recommended to eat a diet rich in vegetables and fruit and to eat only small amounts of cholesterol-containing foods with animal fats and meat. All stress factors should also be reduced. Those affected can also find help in self-help groups and internet forums.

.jpg)



















.jpg)



