The term Hypovolemia refers to a lack of volume in the circulatory system. This means that the amount of blood circulating is decreased. Hypovolemia can lead to life-threatening hypovolemic shock.
What is hypovolemia?
At a Hypovolemia the amount of blood in the bloodstream is decreased. Hypovolaemia is the opposite of hypervolemia. The amount of blood in the human body normally corresponds to seven to eight percent of body weight. A person weighing 70 kilograms therefore has around five liters of blood. The loss of about 750 milliliters of blood is not in the critical range. The first symptoms appear from a loss of 1.5 liters. Loss of more than two liters of blood can be life threatening.
causes
The most common cause of hypovolaemia is bleeding. A distinction can be made between internal and external bleeding. External bleeding comes out of the body, internal bleeding bleeds into the body. Drastic bleeding can result from injury to blood vessels. For example, cuts in large arteries or the rupture of an aortic aneurysm can lead to hypovolemia within a very short time.
Bleeding in the gastrointestinal tract, for example from ruptured ulcers or tumors, can be so massive that it leads to hypovolemia. Fractures of well-perfused bones also lead to severe blood loss. Loss of plasma or fluids also reduces the amount of blood circulating. Loss of fluid occurs with severe and persistent diarrhea or with profuse sweating. Plasma losses, on the other hand, are found in severe inflammation or extensive burns.
Symptoms, ailments & signs

© Sagittaria - stock.adobe.com
As there is less blood circulating in the blood vessels, the blood pressure drops. The blood pressure amplitude is small. The blood pressure amplitude is the difference between the systolic and diastolic blood pressure values. The normal amplitude of blood pressure is around 40 mmHg. To compensate for the low blood pressure, the body increases the pulse rate. Nevertheless, there is usually insufficient blood flow to the periphery. The central venous pressure is decreased, the urine output decreased.
If no fluid or no blood is substituted, sooner or later hypovolemic shock will occur. Hypovolemia and volume depletion shock can be roughly divided into three stages. In the early stages, blood pressure is normal. The skin appears pale and is cool and moist. No other signs of decompensation can yet be seen. In the second stage, tachycardia occurs. This means that the pulse rate is accelerated. The pulse is weak and therefore difficult to feel.
The systolic blood pressure drops to values below 100 mmHg. Urine excretion decreases and patients complain of severe thirst. The neck veins can no longer be seen because they have collapsed due to the lack of fluid. In the third stage there are massive signs of decompensation. The systolic blood pressure is below 60 mmHG, the pulse can no longer be felt. Breathing levels off and becomes faster. Renal function failure with anuria and impaired consciousness occur.
Diagnosis & course of disease
The symptoms of the cause provide the first indications of hypovolemia. Open wounds may be visible, the patients report diarrhea, burns are visible or the pain indicates internal bleeding. A careful anamnesis is therefore mandatory. Symptoms such as cold sweating, sunken veins or a barely palpable pulse also indicate hypovolemia.
The so-called shock index is suitable for estimating the extent of hypovolemia. The pulse rate is divided by the level of the systolic blood pressure value. Values less than one are physiological. A shock threatens around the value one. All values greater than one can be interpreted as an indication of a manifest shock.
Complications
In the worst case scenario, hypovolemia can lead to death. The patient's resilience is considerably restricted by the disease and there is a strong reduction in quality of life and restrictions in everyday life. The low blood pressure can also lead to a loss of consciousness, in which the patient can be injured by a fall or an accident.
Urine excretion is also reduced in the patient. The person concerned often looks pale and exhausted and suffers from a general feeling of illness. Furthermore, there is a revered thirst. Without treatment, the kidneys can be damaged, leading to renal failure. The affected person is dependent on dialysis or a donor organ. Disturbances of consciousness and coordination disorders also occur.
Treatment is carried out with the help of infusions. Furthermore, the patient's volume is increased again in order to avoid consequential damage. There are no complications with early treatment. However, these can occur if the hypovolemia is not treated quickly enough. Organs are irreversibly damaged, which in the worst case can lead to the death of the patient.
When should you go to the doctor?
Symptoms such as tiredness, fatigue, and low blood pressure can indicate hypovolemia. If these symptoms persist for more than two to three days and increase in intensity as the disease progresses, medical advice is required. If you are very thirsty and have impaired consciousness that cannot be traced back to any other cause, you must also be clarified by a doctor. This is especially true if the symptoms occur in connection with an injury in which the person concerned has lost a lot of blood.
If the blood pressure drops at the same time, a doctor must be consulted immediately. Otherwise, it can lead to serious complications. The emergency doctor must be called at the first signs of hypovolemic shock. In any case, the affected person must be examined and treated in a hospital, and hypovolemia can usually be treated well. The prerequisite for this is that the lack of blood in the body is recognized and clarified at an early stage.In addition to the family doctor, a specialist in internal medicine can also be consulted.
Doctors & therapists in your area
Therapy & Treatment
The aim of treating hypovolaemia is to normalize circulating blood volume. This is usually achieved by giving isotonic crystalline or colloidal infusion solutions. Hyperosmolar infusion solutions are also available for particularly rapid volume replacement.
Of course, not only the hypovolemia itself, but also the cause of the volume deficiency must be treated. If blood is lost, the bleeding must be stopped as soon as possible. Bleeding wounds should be covered with a pad if possible. If the bleeding is severe, a pressure bandage is usually applied first. If this does not stop the bleeding, it may be necessary to tie off blood vessels. After this first aid, severe bleeding is usually treated surgically. In addition to these therapies, bicarbonate buffer solutions are used to prevent acidification of the body.
As a result of the reduced blood flow to the kidneys and lungs, hypovolemia can lead to a shock kidney or shock lung. The shock kidney refers to kidney failure as part of the shock process. Any reduction in urine volume during a shock should include a shock kidney.
The shock lung is also known as acute lung injury syndrome. A few days after the actual shock, pulmonary edema with shortness of breath occurs. The skin may also turn blue, restless and confused.
prevention
To prevent hypovolemic shock, you should always ensure a balanced fluid balance. In the case of severe diarrhea or prolonged vomiting, sufficient fluid should always be substituted. Electrolyte solutions from the pharmacy are particularly suitable for this. In addition, a doctor should always be consulted if diarrhea persists, and especially if children have diarrhea.
The same applies to symptoms such as severe stomach or intestinal pain. This pain can hide an ulcer. If this ruptures, it can lead to severe internal bleeding. This can be prevented through early diagnosis and appropriate therapy.
Aftercare
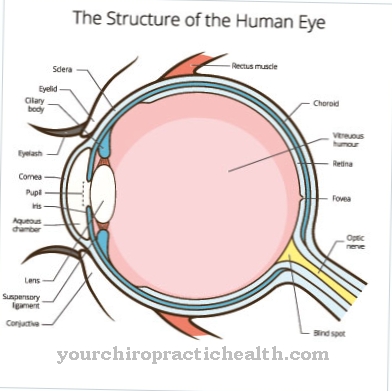
There is no causal cure for hypotrichosis with juvenile macular dystrophy, but with follow-up care, those affected can make their lives more comfortable. It is important to prevent physical harm. The eyesight is often impaired in the sick children. With an early therapeutic approach, the aggravation or blindness can be slowed down and perhaps even avoided.
The attending physician often involves the patient in active therapy and aftercare. The doctors' recommendations make the children feel motivated to consistently keep the treatment appointments. In order to accept the restrictions in everyday life, psychotherapeutic support is advisable.
This type of aftercare is particularly relevant for patients with malformed limbs. Long-term support from psychological carers is just as helpful as targeted physiotherapy. The patient's mobility is maintained through physiotherapy exercises.
Comprehensive measures related to aftercare also help to participate in social life. This is an important point for the children affected and for the whole family. Self-help groups and special care facilities provide the necessary support and offer patients good opportunities to lead a relatively independent life.
You can do that yourself
In the case of hypovolemia, the cause of the volume deficiency must first be treated. If blood is lost, the bleeding must be stopped immediately and the wound covered with a pad if possible. Heavy bleeding should be stopped with the help of a pressure bandage. In severe cases it is necessary to tie off the blood vessels.
If a hypovolemic shock has already occurred, the injured person must be brought into the shock position. Raising the legs allows the blood to flow from the legs into the body and thereby regulate the blood volume in the upper body. The first aiders should also call an emergency doctor.
The medical treatment of hypovolemia can be supported by a few hygiene measures and a change in lifestyle. In the first few days after the operation, the wound must be carefully cared for and carefully monitored. If there are signs of infection or other complications, the person should let the doctor know. The diet should be put together in such a way that any deficiency symptoms as a result of blood loss can be quickly compensated for. Although infusions are usually given in the hospital, a supplementary diet makes sense.




.jpg)

.jpg)





.jpg)