The immunological memory is made up of T and B memory cells and provides the immune system with specific information about certain pathogens. In this way, the immune system can fight diseases more effectively and faster after the initial infection. In autoimmune diseases, incorrect information is presumably stored in the immunological memory.
What is Immunological Memory?

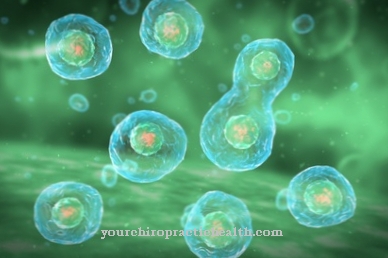
The T memory cells and the B memory cells of the immune system are summarized as immunological memory. Especially the white blood cells (leukocytes) and their subgroup, the lymphocytes, assume immunological functions in the organism of higher living beings.
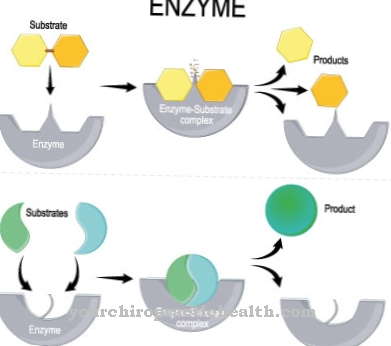
Memory T and B cells are specialized subsets of the T and B lymphocytes. Both B and T lymphocytes are capable of forming antibodies and are part of the adaptive immune system, which reacts to foreign antigens with humoral and cellular immune responses.
B or T cells are activated when they first come into contact with a specific antigen. Most of them then die. The remaining cells can develop into memory cells. When they come into contact with the antigen again, they are activated immediately and "remember" the respective antigen. In a very short time, you trigger the immune reactions you have learned to prevent an infection from breaking out.
There were first speculations about the existence of an immunological memory in the 19th century, when a measles epidemic broke out on the Faroe Islands and protection against a new disease could be observed.
Function & task
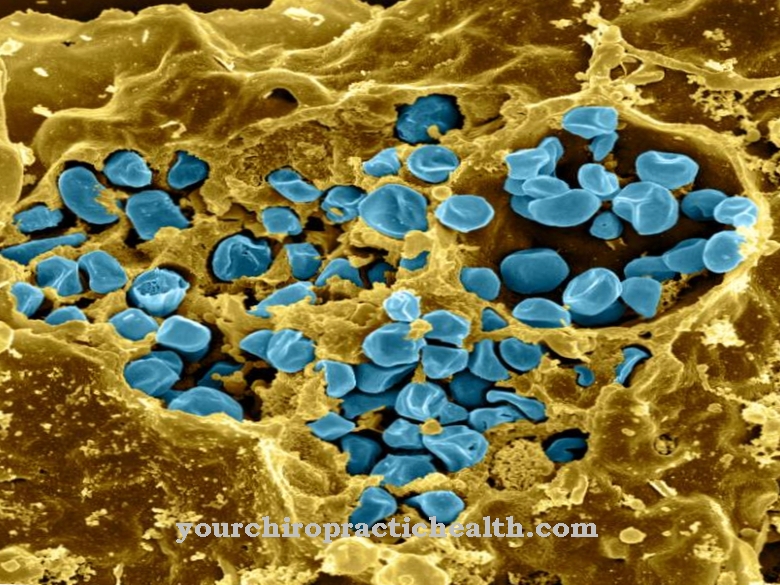
Immune responses are either humoral or cellular. Pathogens in the blood or in the lymph trigger humoral immune responses. Plasma proteins in the form of immunoglobulins are present in the body fluids to combat antigens. The cellular immune response is not controlled by immunoglobulins, but specifically by T lymphocytes. They move in the blood and in the lymph fluid and dock with their receptors on antigen-representing cells in order to trigger cell death.
The activation of T and B cells through contact with a pathogen turns them into memory cells. B memory cells thus form the information store for the formation of antibodies against diseases that an organism has previously suffered from. Every humoral immune response activates B cells that have suitable antibodies on their surface to fight against. The B cells divide after activation. Some of the cells become plasma cells. The remaining B cells transform into B memory cells. When the body comes into contact with the pathogen again and a humoral immune response is required, B memory cells transform into plasma cells at breakneck speed. An antibody reaction is triggered before an infection breaks out.
A similar process takes place with regard to T cells. By stimulating the immune system with an antigen, specific T cells multiply tenfold to one hundredfold. Most of the T cells only have a short lifespan and die preprogrammed cell death after an immune response. Around five percent of the cells survive the immune response. These cells transform into long-lived memory cells and ensure a rapid immune response after repeated contact with the antigen.
The human immunological memory stores information about specific pathogens and makes it available to the organism. Memory cells are supported in survival by eosinophilic granulocytes. Thus, the immune system is adaptive, adaptive and therefore more effective. The information stored in the immunological memory is available to the immune system of the organism for several decades because of the longevity of the memory cells.
You can find your medication here
➔ Medicines to strengthen the defense and immune systemIllnesses & ailments
Autoimmune diseases are anchored in malfunctions and misinformation that are stored in immunological memory. In rheumatism, multiple sclerosis or the intestinal disease Crohn's disease, the body fights itself. In a healthy person, the immune system recognizes certain pathogens as foreign thanks to the immunological memory and knows exactly which antibodies it has to send to fight it. In autoimmune diseases, the immune system is no longer able to differentiate between foreign substances and the body's own substances. Therefore, antibodies are sent against the body's own tissue.
So far, autoimmune diseases are considered incurable. With drugs such as immunosuppressants, the destructive attacks against the body's own tissue can be suppressed, delayed or at least weakened.
Immunological memory has its headquarters in the bone marrow, where the memory plasma cells are made and survive for years. A relatively new approach to curing autoimmune diseases is being discussed with the removal of eosinophils from the bone marrow. Since the granulocytes help the memory cells survive, removing them would drive the cells to death.
Regulating an overactive immune system by temporarily removing granulocytes from the bone marrow could erase the immunological memory that makes up the autoimmune disease. Experience with cancer patients with additional autoimmune diseases shows that immunological memory can actually be erased. Chemotherapy destroyed her entire immune system. It was able to be rebuilt by transplanting its own stem cells. In a majority of the cases, their immunological memory was then erased and they had overcome their autoimmune disease.
Despite the success of this therapeutic option, the erasure of immunological memory is temporarily associated with a high risk of infection and is therefore not approved for the masses. In the future, however, it may be possible to use subtle methods to search for certain memory cells in the body that can be specifically switched off.




.jpg)











.jpg)