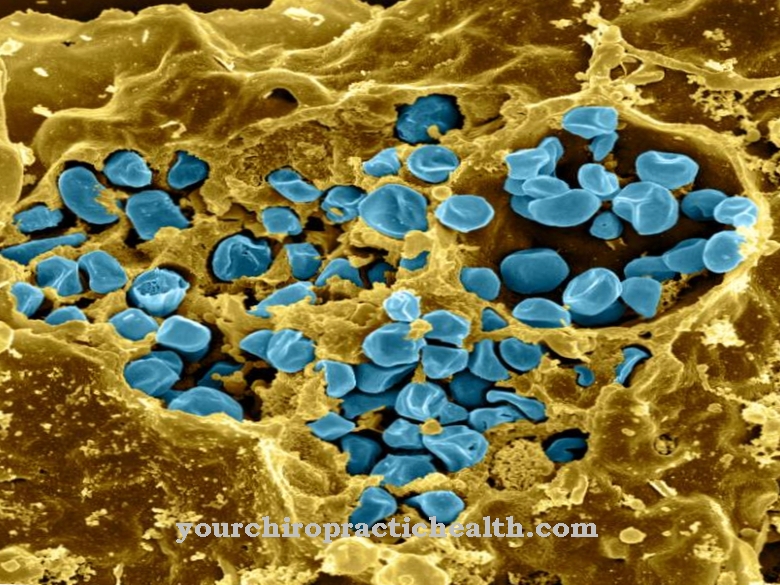
The Impetigo contagiosa is a highly contagious bacterial infectious disease that occurs primarily in newborns and children. In principle, however, the infection can occur at any age. Are synonyms impetigo, Lichen, Ringworm or train. Most often the face and extremities are affected.
What is impetigo contagiosa?

© Syda Productions - stock.adobe.com
The Impetigo contagiosa is one of the bacterial infections of the skin. It is common and highly contagious. While the infection can affect any age, children and newborns are most commonly affected.
There are two forms of impetigo contagiosa that are caused by different bacteria. The small-bubble form is caused by group A beta-hemolytic streptococci. The causative agent of the large-bubble form is Staphylococcus aureus.
The incubation period is two to ten days. There is a risk of infection as long as open, purulent areas of the skin have not healed. During this time, the vesicles and their contents are highly contagious.
causes
The Impetigo contagiosa is transmitted through a smear infection with the named bacteria. The bacteria are also found in the nasopharynx of many healthy people.
The disease occurs when the pathogen penetrates the bloodstream through scratched or injured skin and can destroy tissue there. Therefore, children with neurodermatitis, chickenpox or scabies, for example, are particularly susceptible to impetigo contagiosa.
The bacteria are transmitted through direct contact or contaminated hands (smear infection). They also survive for a long time on glasses or other objects. This means that indirect transmission is also possible if a contaminated object is used by several people. The infection spreads particularly easily in community facilities such as schools or kindergartens.
Symptoms, ailments & signs
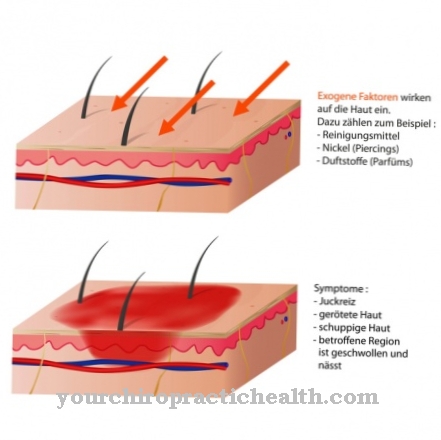
The three forms of impetigo contagiosis manifest themselves through predominantly uniform symptoms. The small, white to reddish blisters on the skin are typical. These skin changes, which are very small in the non-bullous form and therefore hardly visible, burst after a while and yellowish crusts form.
Then there is often an itchiness. The vesicles can appear punctiform or over a large area. If the infestation is severe, a large part of the skin is affected. In impetigo contagiosa with small vesicles, the vesicles are small and filled with pus and, due to their thin skin, burst after a few days. The large-bubble impetigo contagiosa manifests itself as larger skin changes with a thicker skin.
They are clear at the beginning and slowly become cloudy. The blisters burst after one to two weeks and leave the characteristic crust behind. The non-bullous impetigo contagiosa causes few or no vesicles, although yellowish crusts appear. In rare cases, skin changes are accompanied by a fever. The increased body temperature is associated with typical symptoms such as chills and malaise and subsides after a few days.
Diagnosis & course
The doctor can make a diagnosis of the Impetigo contagiosa Make a visual diagnosis, as the rash is typical of the disease. A skin swab (including a swab from the nose and throat) is also possible in order to be able to detect the pathogen in case of doubt. In the differential diagnosis, the doctor rules out a herpes simplex infection.
The rash in impetigo contagiosa is typical. The patient shows golden yellow crusts with a red border, which occur mainly in the area of the mouth and nose and on the hands.
At first, the skin is slightly reddened and blisters filled with fluid or pus form. In the small-bubble form, the wall of the bubble is very thin and bursts quickly. This forms the honey-yellow scab that is typical of the disease.
In large-bladder impetigo contagiosa, the patient can also develop a fever and show swelling of the lymph nodes. The fluid in the vesicles is highly contagious. The crust formation is stronger in the small-bubble form than in the large-bubble impetigo contagiosa.
Eventually the flakes of skin fall off on their own or can be removed by hand. With consistent therapy and compliance with hygienic regulations, the infection usually heals without any consequences.
However, complications can also arise during the illness. The patient can develop post-infectious glumeronephritis, lymphadenitis, or regional lymphangitis.
Complications
Impetigo contagiosa mainly causes discomfort in the extremities and face of the patient. In most cases, blisters form on the skin and the affected person suffers from a severe rash. This rash can be itchy, and blisters filled with pus can also form.
The quality of life of the patient is significantly reduced by impetigo contagiosa and there is often a reduced self-esteem due to the aesthetic restrictions. Not infrequently, those affected also suffer from inferiority complexes and depression. They withdraw from social life and also suffer from severe exhaustion.
Swelling of the lymph nodes and the development of a fever can also occur. The affected person also suffers from a reduced resilience. There are no further restrictions or complications in the treatment of impetigo contagiosa.
This usually takes place with the help of antibiotics and leads to a positive course of the disease relatively quickly. The life expectancy of the patient is not restricted by the disease. However, in severe cases, scars can develop.
When should you go to the doctor?
If the child shows symptoms of a skin disease, he or she should be taken to the pediatrician on the same day. External signs such as pus blisters, yellowish crusts or redness indicate that it is impetigo contagiosa - a disease that must be treated by a doctor in any case. Parents who notice symptoms in their child should consult the dermatologist immediately. This is especially true if the child complains of increasing pain and itching.
At the latest when the vesicles open or even become inflamed, the child needs medical attention. Children who have recently had chickenpox, scabies or who have neurodermatitis are particularly prone to impetigo contagiosa. Parents should see a doctor if any of the above symptoms are associated with any of these conditions. If the discomfort is severe, the child should be taken to hospital. Further treatment is carried out by the dermatologist or an internist.
Treatment & Therapy
The doctor will treat you for possible secondary diseases Impetigo contagiosa in more severe cases, systemically with antibiotics (amoxicillin or flucoxacillin).
For the affected areas of the skin, the doctor also prescribes ointments containing antibiotics such as Fusidic acid, mupirocin or retapamulin. Baths and envelopes with disinfectant solutions are also helpful.
You can find your medication here
➔ Medicines for rash & eczemaOutlook & forecast
With professional treatment, the chances of a cure for impetigo contagiosa are very good. The ringworm often heals spontaneously. Nevertheless, those affected with impetigo contagiosa should not wait to see whether that happens. It is safer to start treatment for the infection and prevent the ringworm from spreading to other areas of the skin. Even with medical treatment, it can take weeks for all signs of lichen to go away.
The affected skin areas later show purulent pustules, which open quickly and leave yellow crusts. This is not only ugly, but also contagious. The infection will therefore spread if the person concerned does not take it seriously enough and spreads germs through misconduct.
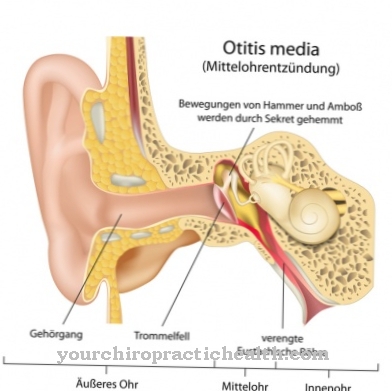
The spread of impetigo contagiosa to other skin areas can certainly lead to secondary diseases. With purulent conjunctivitis (conjunctivitis), the eyes are affected, with otitis media, the ears are affected. In addition, glomerulonephritis can occur if the disease is prolonged. That worsens the prognosis.
Depending on whether staphylococci or streptococci have triggered the impetigo contagiosa, further consequences can occur if the infection is not treated. For example, staphylococci can lead to sepsis or inflammation of the lymphatic system. Untreated streptococcal infections can cause kidney damage such as post-infectious glomerulonephritis.
prevention
Spreading can only be prevented by consistently adhering to all hygienic measures. Under no circumstances should the patient scratch the highly infectious vesicles. In the case of children, parents can therefore also cut their fingernails as short as possible.
Regular hand washing of the patient and of course all contact persons is essential. All items of clothing that the patient has worn and all towels and bed linen used must be cooked at 60 ° C.
This can contain the infection and prevent it from spreading. In order to avoid infection of other people, the patient is only allowed to visit community facilities such as schools or kindergartens again when the infected areas of the skin have completely healed. This is the case when the crusts have completely fallen off.
Aftercare
In most cases of impetigo contagiosa, there are no special follow-up options available to those affected. The earlier the disease is recognized, the better the further course, so that the person affected should ideally see a doctor as soon as the first complaints and symptoms appear. Impetigo contagiosa cannot heal itself.
In most cases, the disease is treated by taking various medications. If antibiotics are administered, the person concerned should not take them together with alcohol, as this would significantly reduce their effect. It is also important to ensure that it is taken regularly and that the dosage is correct.
If anything is unclear or if you have any questions, a doctor should always be consulted first. Furthermore, no special measures are usually necessary. Impetigo contagiosa does not reduce the life expectancy of the person affected. However, the patient should take it easy and rest. Exertion or stressful activities should be avoided in any case, in order not to unnecessarily burden the body.
You can do that yourself
In the case of impegno contagiosis, medical treatment is required in any case. Medical therapy can be supported by some self-help measures and various resources from the household and nature.
The most important measure is to peel off the crusts twice a day. For this, an antiseptic solution is required, which softens the incrustations and thus prevents injuries to the skin. Then the wound can be treated with an antiseptic ointment or a local antibiotic and closed with a fresh bandage. Thorough hygiene must be observed when removing the crusts, otherwise inflammation can occur. If larger skin areas are affected, disinfecting baths with quinolinol or potassium permanganate are recommended. Treatment with antibiotics is necessary in the chronic course.
Both medical preparations and strict hygiene measures help against the itching. Sufferers should wash their hands frequently and thoroughly and not bathe with other family members or the partner. In addition, the fingernails should be trimmed regularly and the towels should be washed hot after use. Those affected should take sick leave for at least one to two weeks. Only when the doctor gives the all-clear can direct physical contact with other people be resumed.

.jpg)


.jpg)











.jpg)