Klebsiella pneumoniae is one of the hospital germs. The bacterium mainly damages people who are already in poor health.
What is Klebsiella pneumoniae?
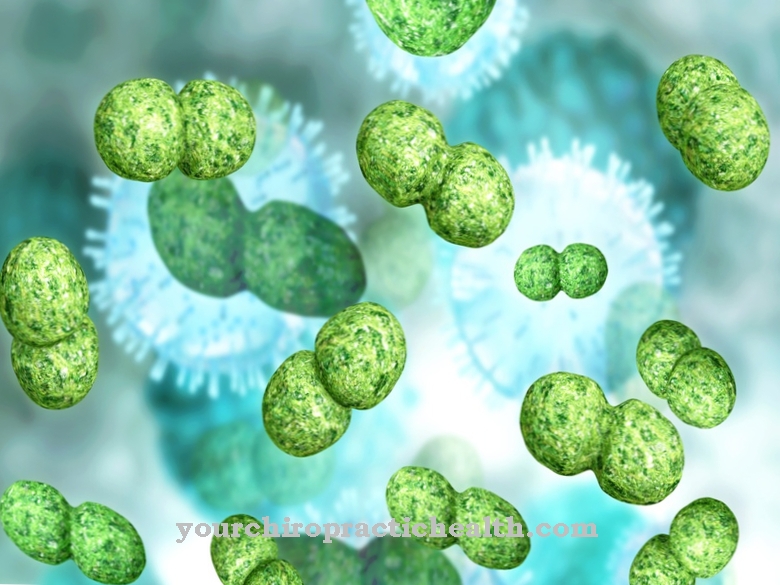
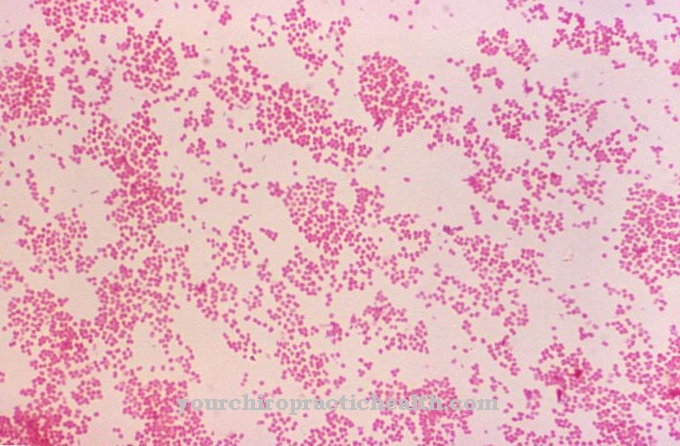
Klebsiella pneumoniae is a gram-negative human pathogenic rod-shaped bacterium that comes from the genus Klebsiella. The bacterium is one of the fast fermenters of lactose and is oxidase negative. It belongs to the Enterobacteriaceae family.
Normally, Klebsiella pneumoniae does not have a dangerous effect on humans. However, if a person's immune system is weakened or if there is an acute infection, the microorganism also shows itself as a pathogen. This primarily results in diseases of the upper respiratory tract, such as pneumonia. In addition to humans, animals can also be affected by Klebsiella pneumoniae.
The genus Klebsiella was named after the German physician Edwin Klebs (1834-1913). Klebsiella pneumoniae was first described in 1883 by the German microbiologist Carl Friedländer (1847-1887). Friedländer determined that the germ was the cause of a rare form of pneumonia, which was called Friedländer pneumonia. The name for Klebsiella pneumoniae at that time was Diplococcus. Furthermore, the pathogens were also Friedlander bacteria called.
In the following years, the scientists divided the bacterial species into three subspecies: Klebsiella pneumoniae, Klebsiella ozaenae and Klebsiella rhinoscleromatis. Klebsiella rhinoscleromatis causes a rhinoscleroma, which is a granulomatous inflammation of the nasal mucous membrane. Pneumonia is also possible due to complications.
Occurrence, Distribution & Properties
Klebsiella pneumoniae is normally found in the intestines of humans and animals, where it belongs to the intestinal flora. There the bacterium does not cause any diseases and is considered harmless. Klebsiella pneumoniae occurs in the body in about a third of the population without causing disease. In addition to the intestine, the oral mucosa is also often populated by the bacterial species.
All Klebsiella species are classified as chemoorganotrophs. Organic substances are broken down by them in order to generate energy. In addition, Klebsiella pneumoniae is facultatively anaerobic. If the bacteria have sufficient oxygen, an oxidative energy metabolism occurs. Organic substances are oxidized to carbon dioxide (CO2) and water if there is no oxygen. Under anoxic conditions, 2,3-butanediol fermentation is used to conserve energy. The main end products are CO2, the alcohol 2,3-butanediol and some acids.
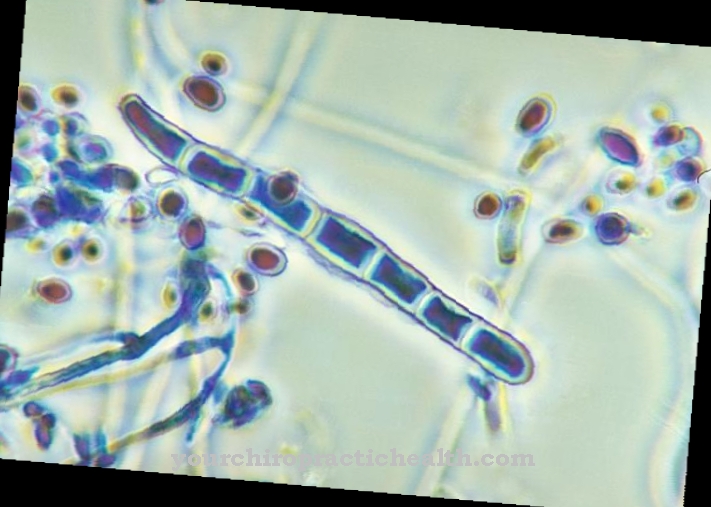
Klebsiella pneumoniae has the shape of a rod. The microorganism does not produce spores. In addition, the bacterium does not have flagella, so it remains immobile. For this purpose, Klebsiella pneumoniae is equipped with fimbriae (fringes or tassels).
A large capsule is a typical feature of the Klebsiella bacterium. This creates a thick layer of slime on crops such as an agricultural plate. If aerobic conditions prevail, there is rapid and pronounced growth.
In order to be able to detect and differentiate Klebsiella pneumoniae, a bacterial culture is normally set up. This can be done in a liquid culture or on a solid selective culture medium such as MacConkey agar. It is important to differentiate Klebsiella pneumoniae from other enterobacteria that are similar to the germ. However, a bacterial culture is considered to be relatively uncertain evidence. In the case of serological detection, the bacterium is identified by means of capsule antigens. Further detection options are a so-called colorful series, which consists of test tubes with several culture media, in which differences in the performance of the metabolism can be recorded.
Illnesses & ailments
Klebsiella pneumoniae only becomes a health hazard under certain conditions. Therefore the bacterium is one of the facultative pathogenic germs. In most cases, it causes nosocomial infections. Klebsiella pneumoniae is responsible for around 10 percent of all Klebsiella infections. People with a weakened immune system are considered to be particularly at risk for a disease. The same applies to newborn babies, as they do not yet have an adequate immune defense.
Since Klebsiella pneumoniae infections usually occur in hospitals, the bacterium is also one of the hospital germs. There is also resistance to antibiotics. Klebsiella pneumoniae is insensitive to the common antibiotics. Even the reserve drug carbapenem is sometimes used in vain. In recent years, the number of infections with carbapanem-resistant pathogens (CRE), such as Klebsiella pneumoniae, has increased significantly, resulting in several deaths. However, as there is no obligation to report CRE infections in Germany, no exact figures are available. The Klebsiella bacteria have also been widespread for some time in other regions such as the USA or the Middle East and cause life-threatening pneumonia.
Particularly problematic is the fact that there are hardly any therapeutic options available to medicine when carpapanems are no longer effective against pneumonia caused by Klebsiella pneumoniae. The only effective remedy is the antibiotic colistin, which can damage nerves and kidneys. So far there are no other effective antibiotics. The bacterium is also naturally immune to numerous penicillins.
Apart from Friedlander's pneumonia, in which the two upper lobes of the lungs become inflamed, Klebsiella pneumoniae can cause other diseases. These include urinary tract infections, meningitis and life-threatening blood poisoning (sepsis). Sometimes the germ also spreads through air conditioning.
Other conceivable diseases caused by Klebsiella pneumoniae are sinusitis (sinusitis), inflammation of the lungs (pleurisy), lung abscess, bronchitis, otitis media, gall bladder inflammation (cholecystitis), inflammation of the bile ducts or bone marrow inflammation (cholangitis) Endocarditis.





















.jpg)


