The Konus Syndrome is a paraplegic syndrome caused by pressure damage to the lower spinal cord at the level of the medullary conus and associated with micturition disorders. Most often the phenomenon occurs as part of a herniated disc. The syndrome is a medical emergency and is an immediate indication for surgical decompression to avoid irreversible damage.
What is Konus Syndrome?

© Henrie - stock.adobe.com
The brain and spinal cord make up the central nervous system. All motor skills are controlled via the nerve tissue located here. The spinal cord in particular plays an important role in controlling movement.
Particularly important in this context are the pyramidal tracts, from which all voluntary and reflex movement commands are transported to the muscular success organs via efferent nerve tracts. Correspondingly, damage to the spinal cord has serious consequences. Lesions in the area of the entire diameter of the spinal cord are called, for example, paraplegic syndrome.
All paraplegic syndromes are associated with paralysis. Depending on the type of spinal cord damage, the symptoms of paralysis are either flaccid or spastic paralysis. The so-called cone syndrome is a cross-sectional syndrome with damage location at the level of the conus medullaris, which affects the spinal cord segments S3 to S5. The main symptoms of the syndrome are incontinence and disorders of sexual function.
causes
The cause of Konus syndrome is compression of the lower spinal cord. Pressure on the medullary conus at the end of the caudal spinal cord causes the disorders associated with the syndrome. More precisely, the sacral spinal cord segments from S3 to S5 are primarily affected by the associated compression.
The coccygeal spinal cord at the level of the lumbar vertebrae can also be affected. In most cases, cone syndrome is the result of a herniated medial disc. Circulatory disorders or even tumors are more rarely responsible for the compression of the corresponding spinal cord segments.
The syndrome has also been reported in cases where the medullary conus is inherently attached to its surrounding structures. In such a case, however, it is more of a tethered cord syndrome than a cone syndrome, which damages the conus medullaris during growth. In almost all cases, the cone syndrome is associated with the so-called kauda syndrome and is sometimes referred to in this context as the cone-kauda syndrome.
Symptoms, ailments & signs
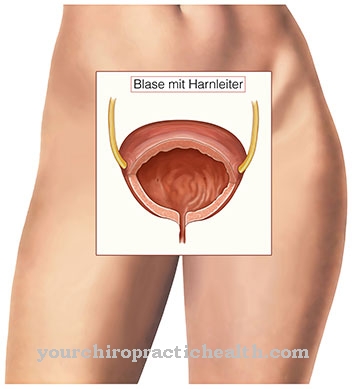
Like all other paraplegic syndromes, cone syndrome is primarily associated with movement disorders. In the case of cone syndrome, this mainly concerns movement disorders of the bladder and anus sphincter muscles. The chair can often no longer be held by the patient. The same goes for urine.
Micturition disorders such as permanently dripping urine are a key symptom of the syndrome. An overflow incontinence, in which the patient's bladder is constantly full, but cannot be emptied at will, can also be considered a micturition disorder. In most cases, there are no movement disorders in the early stages.
At the beginning, the cone syndrome usually manifests itself in what is known as breeches anesthesia, which is characterized by symmetrical sensory disturbances on the inner back of both thighs. This area of skin is supplied by the nerves in segments S1 to S3. Men in particular often suffer from erectile dysfunction or ejaculation disorders in the later stages of cone syndrome.
As a rule, the compression causes at least slight pain in the hip area, since sensitive nerves are also damaged by the pressure on the lower spinal cord. Paralysis of the legs usually does not occur.
Diagnosis & course of disease
The doctor makes the diagnosis of cone syndrome using medical history and imaging. Patients' anus is essentially flaccid because the sphincter muscle is not working adequately. As part of the diagnosis, a failed anal or bulbocavernosus reflex can indicate the cone syndrome. Patellar and Achilles tendon reflexes are preserved in isolated cone syndrome.
CT or MRI can be used as diagnostic and cause-clarifying imaging. For example, the imaging may show a herniated disc. For patients with Konus syndrome, the prognosis depends largely on the time of diagnosis. If the compression continues for too long, the affected nerves die irreversibly.
Complications
The cone syndrome is a very serious and dangerous condition for the body of the person concerned. If treatment is not started immediately, it can usually lead to irreversible consequential damage and paralysis of the entire body. The affected person suffers from micturition disorders and from paralysis and tingling sensations.
The quality of life is considerably restricted and reduced by the cone syndrome. It is not uncommon for this to lead to movement disorders, so that the patient may also be dependent on a wheelchair. The function of the bladder is also impaired, so that urination can no longer be properly controlled. It is not uncommon for depression and other psychological complaints or moods to occur.
Sensory disorders can occur all over the body, which have an extreme effect on everyday life. The genitals are usually affected by erectile dysfunction. The quality of life of the patient is drastically reduced by the Konus syndrome. It is not uncommon for severe pain to occur in the hip. Treatment for Konus syndrome must be immediate.
Complications are most common when delayed treatment is initiated. This can lead to irreversible damage, so that the person affected suffers from the consequences and paralysis for his entire life. No general statement can be made about the limitation of life expectancy.
When should you go to the doctor?
Konus syndrome is always a medical emergency. Treatment must be started immediately if symptoms such as paralysis or numbness in the legs are noticed. After the initial treatment by the emergency doctor, the patient must be examined in a specialist clinic. Long-term therapy is planned individually depending on the severity of the paraplegia and carried out by various specialists. People who suffer from Konus syndrome must consult their doctor closely. The paraplegic syndrome can be treated well, however, as the condition progresses, various complaints can arise that require individual treatment.
Patients who suddenly notice signs of movement disorders in the bladder and anus sphincters should inform their doctor. Unusual sensory disturbances or pain should also be clarified if they occur suddenly and a medical complication is suspected. The Konus syndrome significantly limits the quality of life, so those affected often also need therapeutic support. If depressive moods or other problems become noticeable, it is best to inform the doctor. They can examine the patient to rule out an organic cause and call in a therapist if necessary.
Treatment & Therapy
Konus syndrome is always a medical emergency that requires immediate intervention. The longer the pressure on the lower spinal cord, the more likely it is that the nerves will be permanently damaged. After the diagnosis has been made, surgical decompression is carried out as soon as possible.
Conservative drug measures are not suitable for treatment. The cause of the existing disorders must be eliminated, in this case the pressure condition near the spinal cord. In individual cases, a so-called nucleoplasty is used to relieve the lower spinal cord. This procedure is a minimally invasive treatment for the therapy of herniated discs.
In this case, the intervention takes place under local anesthesia. During the procedure, the surgeon works with a special probe that is inserted into the spinal cord. In certain circumstances, patients may require specific physiotherapy after the procedure. The symptoms caused by the compression usually improve as soon as the spinal cord is relieved.
However, the initial physiological state is usually not fully restored through the relief. Physiotherapeutic measures are particularly important in the case of cone syndrome, which was recognized and corrected late.
You can find your medication here
➔ Medicines for painOutlook & forecast
The prospect of a cure in Konus syndrome depends on the speed of medical treatment. Since the illness is an intensive care emergency, an ambulance service must be alerted as soon as possible. In addition, for a good prognosis, first aid measures must be taken by those present. If emergency care or medical care is denied, the prospect of recovery deteriorates immensely. Normally it can no longer be achieved in the further course of life. The damage suffered to the organism is irreversible and usually causes consequential damage. The later extensive therapy can be initiated, the more severe the long-term effects of Konus syndrome.
For many patients, despite all efforts, it is not possible to achieve freedom from symptoms, since full care was not provided immediately after the triggering event. Paralysis or restrictions on movement are often lifelong. In addition, psychological sequelae can be expected due to the emotional stress of the disease.
In addition, initiated therapies, the administration of medication and invasive treatments can trigger complications or side effects. These lead to the need to optimize the treatment plan and can delay the healing process. Months or years after the triggering event, many patients report impaired quality of life due to the symptoms that are still present.
prevention
Since the herniated disc is the most common cause of cone syndrome, the same preventive measures apply to the prophylaxis of the syndrome as for herniated discs. For example, back training or regular visits to a back school have proven to be an effective preventative measure in connection with herniated discs.
Aftercare
In the case of Konus syndrome, the follow-up measures are very limited in most cases. As a rule, the disease cannot be completely treated either. First and foremost, the person affected depends on a quick diagnosis so that there is no further paralysis of the body. In many cases, the paralysis itself can no longer be reversed, so that in these cases there are no longer any follow-up measures available to the affected person.
Most of those affected are therefore dependent on the help of other people in their lives and need support in their everyday lives. Above all, the help and care provided by your own family and friends has a very positive effect on the further course of the disease. Depression or other mental disorders can often be alleviated or even prevented.
Physiotherapy measures are often also necessary for cone syndrome. The person affected can repeat the exercises at home and thus accelerate the healing process. Further follow-up measures are usually not possible. However, the syndrome usually does not reduce the life expectancy of those affected.
You can do that yourself
The cone syndrome is always a medical emergency. As soon as the first signs of the paraplegic syndrome appear, an ambulance service must be called. Until this arrives, first aid measures must be carried out or the person concerned should lie down and try to breathe calmly.
After the operation, the person concerned has to take it easy. Exercise and other physical activity should be avoided for the first few days. After a week, you can start again with gentle sport in consultation with your doctor. If the cone syndrome is only recognized at a late stage, the damage that has already occurred must be corrected. This is achieved primarily through physiotherapeutic measures that can be supported by the person affected by individual training. The doctor will refer the patient to a suitable physiotherapist for this purpose.
Identifying and correcting the cause is an important treatment step. Many patients with Konus syndrome are overweight or work in an occupation that puts a lot of strain on the back. These triggers must be found and remedied as quickly as possible. This can be achieved by changing jobs, changing lifestyle habits or accompanying therapy. Regular back training or attending a back school can also alleviate the symptoms and avoid a new cone syndrome.

.jpg)
.jpg)

.jpg)



















.jpg)

.jpg)
