The craniodiaphyseal dysplasia is a congenital skeletal disease associated with hyperostosis and sclerosis of the facial skull. The cause is a genetic mutation in the genes that inhibit bone structure. Therapy is symptomatic and focuses on stopping the disease from progressing.
What is craniodiaphyseal dysplasia?

© crevis - stock.adobe.com
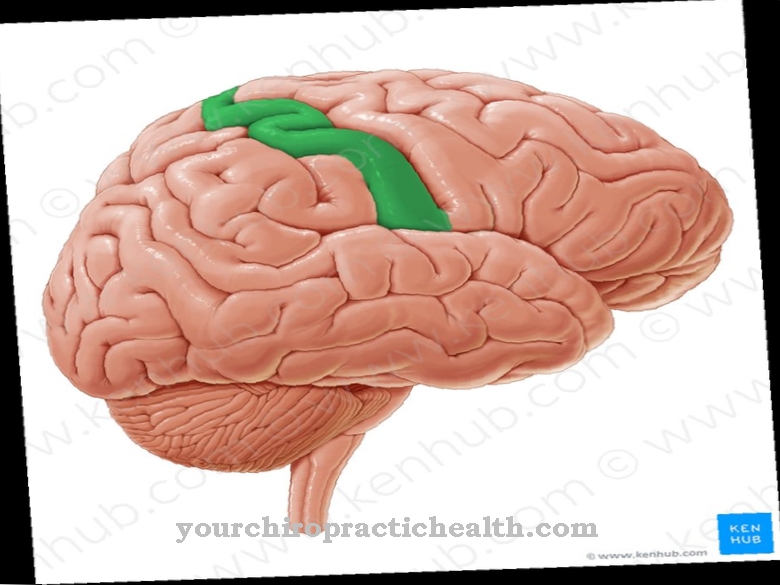
In hyperostoses, the bone substance increases in a pathological way. The hyperostosis of the skull is a group of diseases that is related to such an increase in bone substance in the area of the skull. As craniodiaphyseal dysplasia is characterized by a congenital hyperostosis of the skull and is a skeletal disease.
The Australian doctor John Halliday first described the disease in the middle of the 20th century. The frequency is given with a prevalence of less than one case in 1,000,000 people. This makes skeletal disease an extremely rare dysplasia of the skull.
The complex of hyperostosis and stenosis of the facial and cranial bones has now been traced back to a genetic cause. Due to the few documented cases so far, not all connections between the disease have been conclusively clarified. For this reason, the therapy options are also limited at the moment.
causes
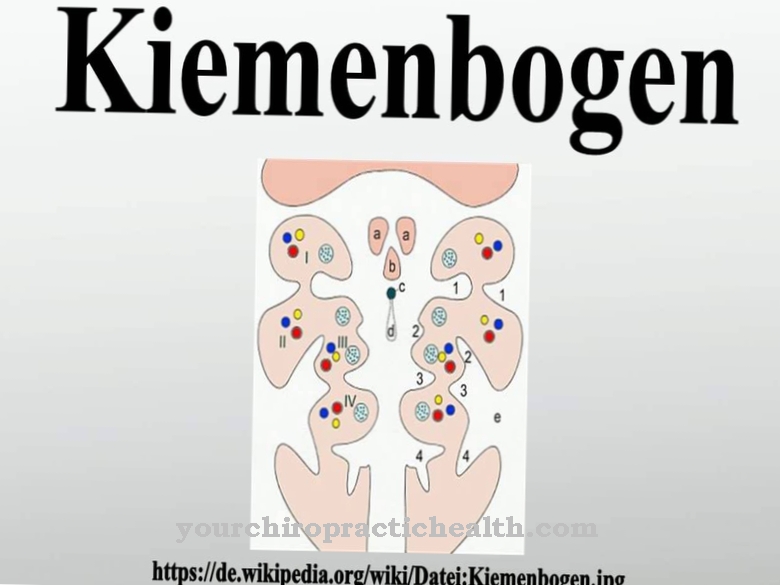
In a large number of cases, craniodiaphyseal dysplasia does not occur sporadically, but with familial accumulation. Both the autosomal recessive and the autosomal dominant mode of inheritance have been identified as the mode of inheritance for the disease. The autosomal dominant form of the disease is based on a new mutation in the SOST gene. The gene is located at location 17q21.31 and is considered to be one of the most important inhibitors of bone formation.
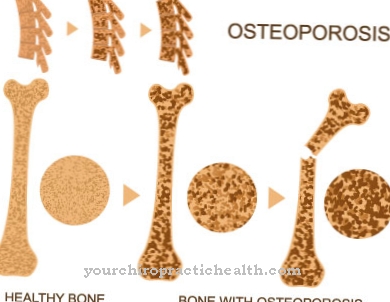
The mutation of the SOST genes is responsible for a large number of hereditary bone diseases, such as VDB. In the event of a mutation, the gene can no longer fulfill its inhibitory functions and the bone structure sprawls. This fundamentally differentiates hyperostosis of craniodiaphyseal dysplasia from other hyperostoses.
Most of these diseases are based on a dysfunction of the osteoclasts or osteoblasts. The genetic disposition is considered to be proven in connection with the disease. What other factors play a role in the onset of the disease has not been conclusively clarified.
Symptoms, ailments & signs
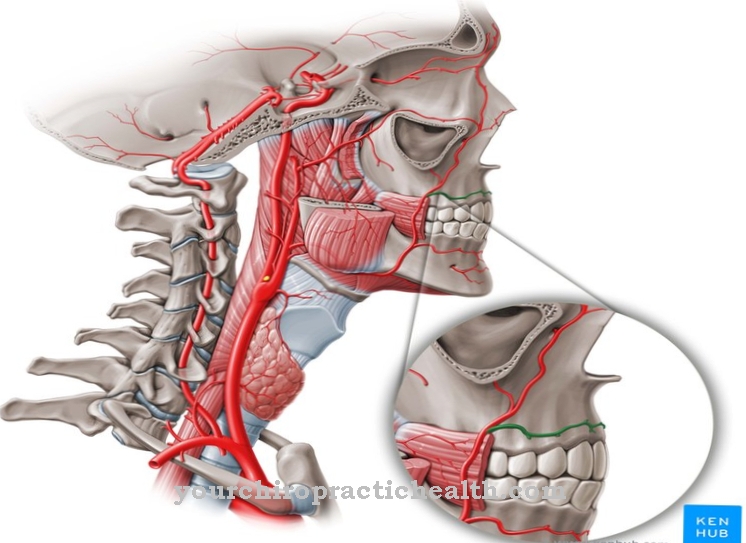
The clinical picture of craniodiaphyseal dysplasia is characterized by various clinical criteria that are already manifested in infancy. Affected infants usually have heavily obstructed nasal passages, which can cause them problems breathing. In the later course of the disease, in most cases there is complete obstruction of the nasal passages.
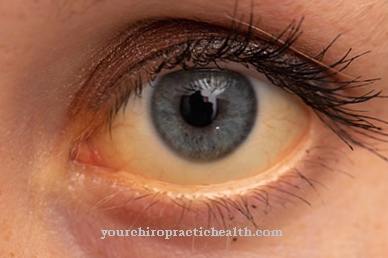
Often the patient's tear ducts become blocked after this phenomenon. On the lower jaw of most of those affected, gradually growing nasal bulges of bony substance form. The hyperostosis of the facial skull progresses and develops into leontiasis ossea. In most cases, the patient's tooth development is disturbed or delayed. The interior of the skull narrows as the disease progresses.
The constrictions also affect the foramina and cause consecutive optic atrophy. This can be accompanied by symptoms such as hearing loss and more or less severe headaches. In some cases, as the interior of the skull becomes increasingly narrow, the patients also suffer from seizures. The shafts of the long tubular bones widen increasingly.
Diagnosis & course of disease
The earliest possible diagnosis and subsequent therapy improves the prognosis of patients with craniodiaphyseal dysplasia considerably. The doctor presumably suspects the hyperostosis from a visual diagnosis. Imaging procedures are considered the most important diagnostic tool. For example, an X-ray shows extreme hyperostosis and sclerosis of all skull bones.
The collarbones or ribs may appear dilated in the imaging. The missing diaphyses on the long bones stand out clearly. A delimitable, non-thickened cortex also fits into the clinical picture. In terms of differential diagnosis, a distinction must be made from diseases such as Engelmann syndrome. Molecular genetic analyzes are particularly suitable for such a differential diagnosis. The Engelmann syndrome shows changes in the TGFB1 gene on mutation analysis, while the craniodiaphyseal dysplasia affects the SOST gene.
Complications
Craniodiaphyseal dysplasia is a rare, genetically determined skeletal disease. The symptom manifests itself directly on the facial skull through a strong increase in bone substance with accompanying sclerosis. The genetic mutation is already evident in infancy based on the shape of the skull and incorrectly laid nasal passages, which can cause threatening breathing problems.
The resulting consequences of craniodiaphyseal dysplasia bring the affected patient numerous life-limiting complications from infancy. If there is no timely clinical intervention, the excess bone growth will progress. The interior of the skull narrows and the rows of teeth do not form adequately. The thickening bone material constricts the ear canal and there is a risk of hearing impairment and even hearing loss.
There is an increasing lack of space in the cranial cavity, and bone deposits penetrate the brain. Severe headaches, seizures, facial paralysis and epilepsy arise as well as a reduction or regression of the mentally acquired skills. Parents whose children are affected by craniodiaphyseal dysplasia should therefore seek clinical measures at an early stage.
After the imaging examination, the differential diagnosis takes place within the scope of the given possibilities. There is currently no basic therapy for craniodiaphyseal dysplasia. Attempts are made to curb the uncontrolled progression of bone growth and its consequences. Various medications as well as a calcium-reduced diet from infancy onwards will help the sufferer to reduce the symptoms.
When should you go to the doctor?
Craniodiaphyseal dysplasia is often diagnosed immediately after birth. If this is the case, the responsible doctor will inform the parents immediately and then initiate treatment directly. If the dysplasia is less pronounced, the diagnosis is made by the parents. A doctor visit is indicated if the newborn has difficulty breathing or watery eyes. External abnormalities such as the typical malformations on the face and teeth also indicate a disease that needs to be clarified and treated.
Parents who experience signs of hearing loss or seizures in their child should see a doctor. The same applies if the child complains of headaches frequently or gives the appearance of severe pain. During treatment, the child must be presented to a doctor regularly. This will ensure that the recovery goes without complications. Because craniodiaphyseal dysplasia is associated with a range of symptoms, therapy can take months or even years. The general practitioner will consult other specialists for this purpose, always depending on the symptoms and complaints. Typically, neurologists, internists, ear specialists, surgeons, physiotherapists and psychologists are involved in the treatment.
Treatment & Therapy
A causal therapy for patients with craniodiaphyseal dysplasia does not yet exist. Such a therapy may be conceivable in the future through gene therapy approaches. At the moment, however, the disease can only be treated symptomatically. The main goal of all therapeutic measures is to stop the excessive bone growth. There are various steps to take.
The progression of the disease can, for example, be stopped with medication. Calcitriol and calcitonin are mostly used as drugs. Since the bone structure is dependent on calcium, a calcium-reduced diet can also make sense. This particular diet should be used in the long term and ideally accompany the patient's entire life.
The drug treatment of patients with the artificial glucocorticoid prednisone has also shown positive effects. The earlier therapy is started, the more promising the prospect. With extremely early treatment, hyperostosis can be brought to a standstill in the first years of life. In this way, the subsequent symptoms are drastically reduced.
Under certain circumstances, surgical corrections can also be made as part of the therapy. However, such corrections usually make little sense before the course of the disease has been brought under control.
Outlook & forecast
In congenital but very rare craniodiaphyseal dysplasia, there is an irreparable genetic mutation. Therefore, the prognosis for those affected is not very good. The medical professionals can only try to treat the symptoms and sequelae of the increased bone growth in the head area. Therapy can only delay the course of the disease. In craniodiaphyseal dysplasia, the increase in bone substance is unstoppable.
Since today's therapy options cannot reverse the underlying mutation in the embryo stage, other generations of those affected will suffer from it. A familial accumulation is noticeable in craniodiaphyseal dysplasia. The symptoms associated with craniodiaphyseal dysplasia can already be seen in the infant. Since all bone adhesions take place in the skull area, the upper respiratory tract as well as hearing or vision are affected by them.
In addition, the interior of the skull is increasingly affected by bone formation. This limits the therapeutic approaches for the subsequent complaints. The earlier the diagnosis can be made, the better the long-term prognosis. A low-calcium diet will inhibit increasing bone growth. In addition, appropriate medication and prednisone can be administered as early as infancy.
An interdisciplinary treatment strategy achieves the best results. Surgical intervention in craniodiaphyseal dysplasia only makes sense if the progression of the disease has been successfully contained.
prevention
So far there are no preventive measures for craniodiaphyseal dysplasia. The disease is a genetic disease that is associated with a familial disposition. Therefore, only molecular genetic counseling can be used as a kind of preventive measure.
Aftercare
In most cases, the person affected has very few follow-up measures available. In some cases, this can even be completely limited, so that the person affected is dependent on purely symptomatic treatment of the disease. Self-healing cannot occur because it is a genetic disease.
Therefore, if the person concerned wants to have a child, they should have a genetic examination and advice carried out so that the disease does not recur in the children. The treatment itself is usually carried out with the help of various drugs that can permanently alleviate and limit the symptoms. It is always important to ensure that it is taken regularly, whereby the correct dosage must also be observed.
In the case of children, parents in particular should check that they are taken and used correctly. Regular checkups by a doctor are also necessary in order to permanently check the condition of the disease. Most malformations can be corrected through surgical interventions. Many of those affected are also dependent on psychological support from their own family in their everyday life, which has a positive effect on the further course of the disease. As a rule, this disease does not reduce the patient's life expectancy.
You can do that yourself
In the case of craniodiaphyseal dysplasia, the affected patient has only limited effective measures available that have a positive effect on the course of the disease. First and foremost is an appropriate therapy of the craniodiaphyseal dysplasia by a team of specialists. The disease begins to manifest itself in infancy, so that it is primarily the parents who contribute to the quality of life of the children concerned. In the case of any inpatient stays of the child's patients, it often makes sense if the parents are present in the hospital and the child receives emotional support as a result.
In the course of the disease, there are often disturbances in the development of the teeth, so that the patients are often dependent on orthodontic therapy. Your own cooperation is also required when it comes to wearing braces. There is also evidence that a low-calcium diet can curb the progression of craniodiaphyseal dysplasia. Here, too, the patients have considerable leeway with regard to their cooperation and thus their quality of life.
Due to the breathing problems, the patients forego certain types of sport, but also practice strengthening exercises at home with a physiotherapist if this is medically permitted. Children with craniodiaphyseal dysplasia receive adequate education in special schools.



.jpg)


.jpg)