Leishmania tropica belong to a large group of flagellated protozoa that live intracellularly in macrophages in skin tissue and require the host change between sand fly or butterfly mosquito and vertebrates for their distribution. They are the cause of cutaneous leishmaniasis, also known as an oriental bump, which is mainly found in southern Europe and in Asian countries. The protozoa know how to survive phagocytosis when they penetrate the bloodstream and how to multiply intracellularly in macrophages in the blood.
What are Leishmania tropica?
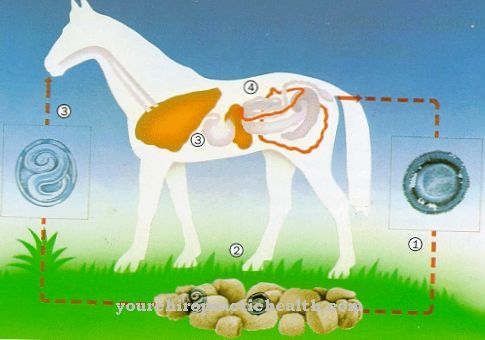
The flagellated protozoa Leishmania tropica form a subspecies of the genus Leishmania and are also known as Hemoflagellates designated. They need a host change between humans or other vertebrates and the sand fly (Phlebotomus) or the butterfly mosquito (Nematocera) for their distribution.
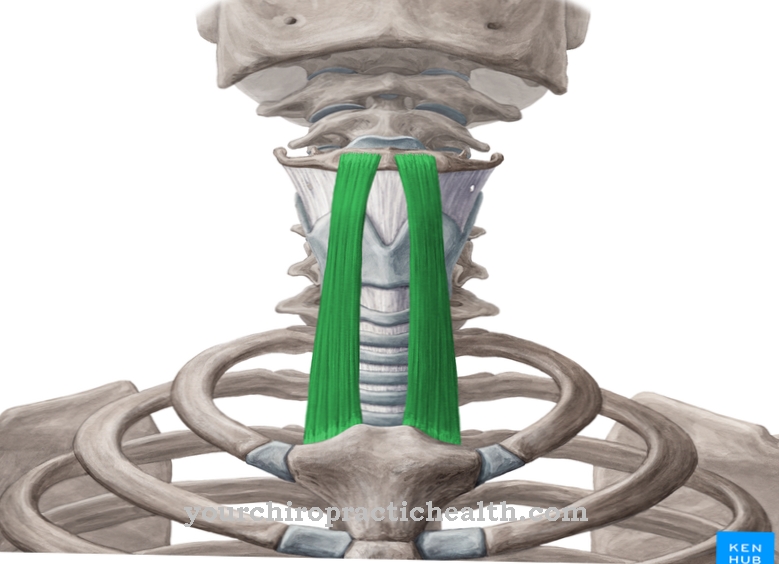
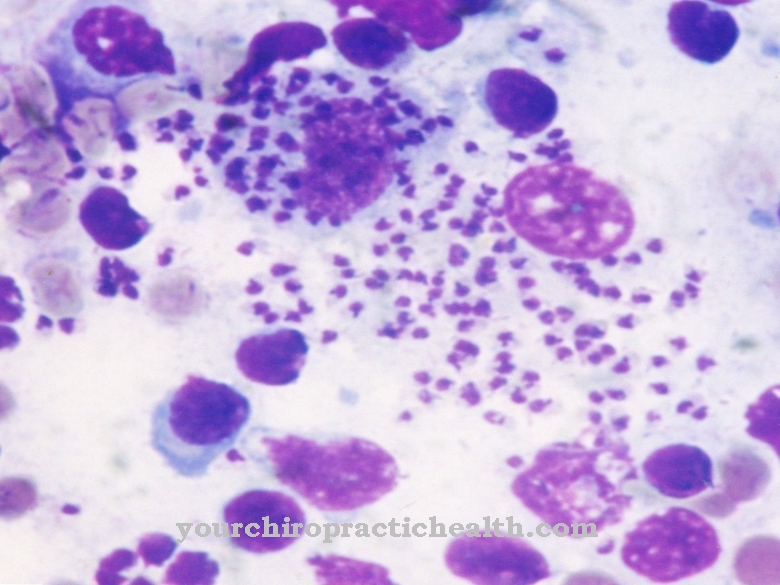
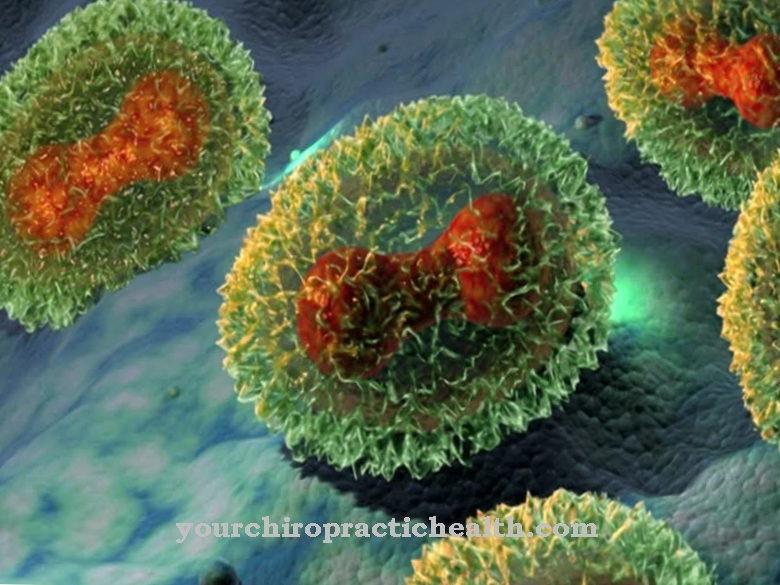
With the change of host, there is always a change between the flagellated (promastigote) and the non-flagellated (amastigote) form of the pathogen. Promastigote pathogens mature in the infected mosquito and use their flagella to actively move to the mosquito's biting apparatus. When the mosquito bites a blood vessel in humans or another host animal, the flagellated pathogens get into the surrounding tissue. They are recognized as hostile by the immune system and are therefore phagocytosed by polymorphic neutrophils (PMN).
Leishmania tropica survive phagocytosis and are initially protected intracellularly. Their actual host cells, the macrophages, reach them after apoptosis of the PMN and renewed phagocytosis - in this case by macrophages. They transform into the amastigote form intracellularly within the macrophages and can multiply through division.
After the pathogen has been released again in the blood, a non-infected or an already infected mosquito can take up pathogens through its proboscis, which are converted back into the amastigote form in the mosquito, so that the cycle is closed.
Occurrence, Distribution & Properties
Leishmania tropica is particularly widespread in countries in West and Central Asia. Endemic occurrences are found in a strip from Turkey to Pakistan, in parts of India, in Greece and in some areas of North Africa. The parasite is only infectious if it is introduced directly into the bloodstream in the flagellated form. The infection occurs naturally through the bite of infected sand or butterfly mosquitoes.
The pathogens are located in the mosquito in the immediate vicinity of the mosquito's suction apparatus. They are washed out with the anticoagulation secretion that the mosquito expels into the stab wound to prevent blood clotting and transported directly into the surrounding tissue. In the tissue, they are captured and phagocytosed by the first wave of immune defense against pathogens, the polymorphic neutrophils, but to a large extent they know how to survive phagocytosis because they produce chemokines that prevent the PMN from releasing their proteolytic substances .
In addition, the flagellated form of the pathogen is able to secrete chemokines, which suppress certain chemokines in neutrophils, which normally also attract other leukocytes such as monocytes and NK cells. By releasing an enzyme that increases the mean survival time of neutrophils from normally a few hours to two to three days, the pathogens can “wait” for macrophages, their final host cells, to appear.
They actively support their host granulocytes in the release of chemokines that attract macrophages. Apoptosis, the programmed and ordered cell death of the PMN, stimulates the macrophages to phagocytosis of the apoptotic cells without releasing their proteolytic substances. The amastigotic Leishmania tropica can thus be absorbed by the macrophages together with the fragments of the granulocytes undamaged and undetected and are now intracellularly safe, so to speak. In the macrophages, the pathogens change from the promastigote to the amastigote form and multiply through cell division.
Illnesses & ailments
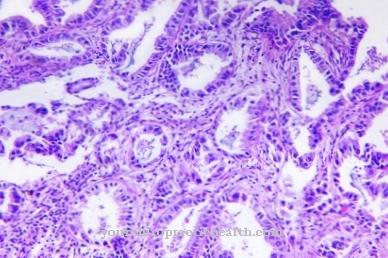
Leishmania tropica causes a cutaneous form of leishmaniasis. The pathogen is transferred to the skin tissue through the bite of an infected sand fly, so that the symptoms of the disease show up after an incubation period of two to eight months on average. In exceptional cases, the incubation period can be considerably longer, up to several years.
Leishmaniasis tropica leads to dry, keratinized skin bumps that are painless and do not itch. If left untreated, the skin bumps usually heal on their own after 6 to 15 months, but sometimes leave behind disfiguring scars. Once the disease has healed, there is usually lifelong immunity.
In rare cases, recurrent (recurring) cutaneous leishmaniasis can occur after one to 15 years. The recurrent form of the disease usually manifests itself in multiple papules, which slowly enlarge at the irregular edges and slowly keratinize and heal from the center. There are relatively few pathogens in the papules. In contrast to visceral forms of the disease (which affect the intestines), cutaneous leishmaniasis tropica is usually more harmless, but usually leaves behind unsightly scars.
Few systemically acting antibiotics and also a locally applied antibiotic are available for treatment. Neither vaccination nor other direct preventive measures to prevent infection are non-existent. The best protection is to use a mosquito net at night in vulnerable areas and apply mosquito repellent during the day.





.jpg)





.jpg)





.jpg)