The Leydig intermediate cells are located between the seminiferous tubules of the testes and produce the male sex hormone testosterone. They are therefore responsible for the secondary sexual characteristics of men and the maintenance of all sexual functions.
What are the Leydig Intermediate Cells?
The Leydig intermediate cells were named after their discoverer Franz von Leydig. They are located in the interstitial space of the testes and make up about 10 to 20 percent of the testicle mass. Their job is to produce the sex hormone testosterone. Testosterone production has two peaks.
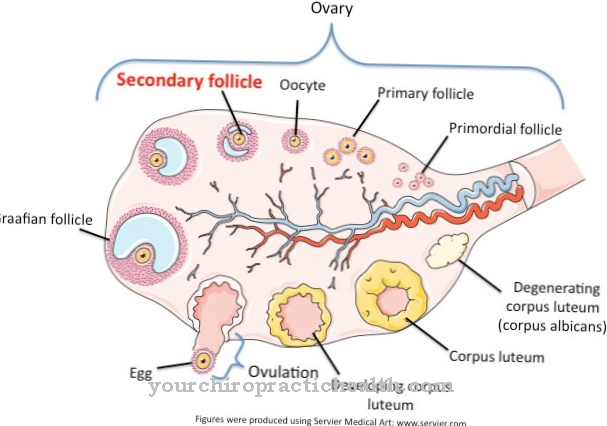
The Leydig cells are stimulated by the pregnancy hormone chorionic gonadotropin from the eighth week of pregnancy to produce testosterone. This is where the male sexual characteristics develop. After they have differentiated, no more testosterone is produced from the sixth month of pregnancy. The second phase of hormone production begins with puberty. The so-called Leydig cell stimulation test is carried out to identify testicular tissue. The tissue to be examined is mixed with the human chorionic gonadotropin. If Leydig interstitial cells are present, testosterone is produced, which can then be detected.
Anatomy & structure
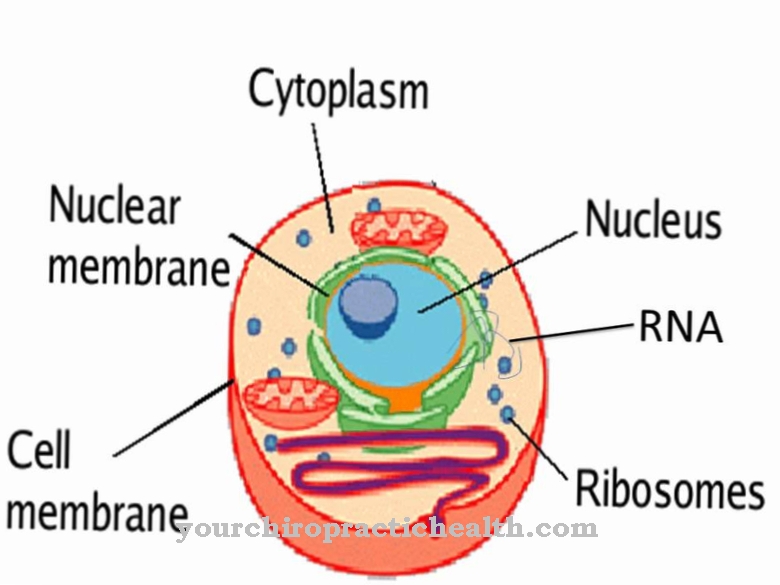
As already mentioned, the Leydig interstitial cells are the most important cell type in the testes. They are found between the tubules in the interstitium and are large, acidophilic cells. Their nucleus is light and rounded. There are many mitochondria in their cells. They are arranged in groups between the seminal canals of the testes. Mostly they are located near the capillaries. The cells are also characterized by the presence of lipid droplets and a large amount of endoplasmic reticulum.
That suggests the production of steroid hormones. In addition to testosterone, dihydrotestosterone (DHT), dihydroepiandrosterone (DHEA) and estradiol are also formed there. In the cytoplasm, so-called Reincke crystals from crystalline protein deposits sometimes occur. The meaning of the Reincke crystals has not yet been clarified. However, they appear to be waste products. The sperm production stimulated by testosterone takes place in the testicular canals. They are protected by Sertoli cells and separated by testicular connective tissue in which the Leydig cells are located.
Function & tasks
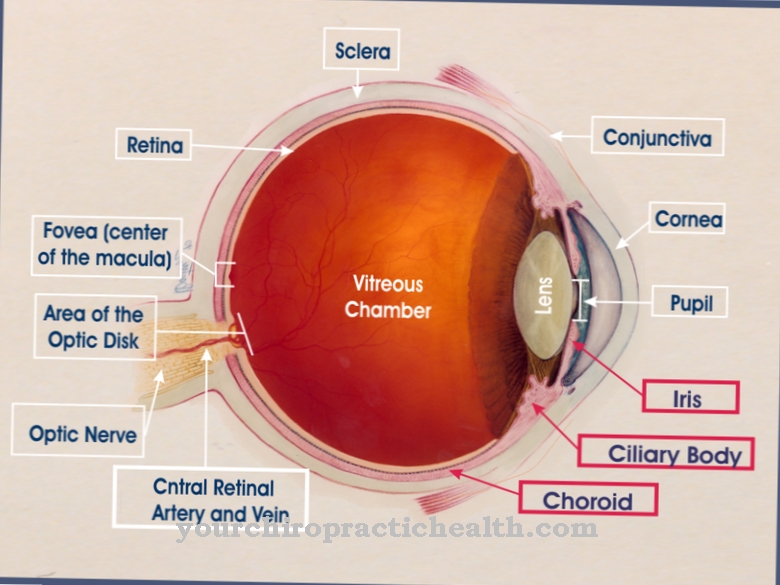
The most important function of the Leydig interstitial cells is to produce testosterone along with a small amount of other sex hormones. The starting substance for hormone synthesis is cholesterol. Testosterone reaches the sexual organs, skin and prostate via the blood. There it is converted into dihydrotestosterone. The female sex hormone estradiol is produced from testosterone in adipose tissue and the liver. Therefore, overweight men often experience a certain feminization, which can also enlarge their breasts.
Testosterone primarily determines the development and function of the male sexual organs as well as the maturation of sperm. It also promotes growth, influences the body structure, the type of hair, the activity of the sebum glands or the size of the larynx. During puberty, therefore, male adolescents often get acne due to the increased sebum production. The normal sex drive and potency in men are dependent on testosterone. It is also responsible for increased blood formation and muscle building. That is why it is often misused as a doping agent. Last but not least, testosterone often creates a certain aggressiveness, which is viewed as a male trait. The production of testosterone in the Leydig interstitial cells is controlled by the hypothalamus and pituitary gland.
When there is a higher need for testosterone, the hypothalamus produces the hormone gonadotropin-releasing hormone (GnRH). This hormone in turn stimulates the pituitary gland, especially the anterior pituitary gland, to produce the regulating hormones FSH (follicle-stimulating hormone) and LH (luteinizing hormone). LH then stimulates the intermediate Leydig cells to produce testosterone. In conjunction with FSH, testosterone now promotes the development and maturation of sperm. In the context of negative feedback, the production of GnRH, FSH and LH is stopped when there is enough testosterone. This feedback is reported to the hypothalamus and pituitary gland by the substance inhibin formed in the Sertoli cells. The Leydig intermediate cells then reduce testosterone production again.
Diseases
The production of testosterone can be disrupted in the Leydig cells. Usually this is an underproduction. This reduced testosterone production is known as hypogonadism. A distinction must be made between primary and secondary hypogonadism. In primary hypogonadism, the Leydig intermediate cells are unable to produce enough testosterone or at all because of pathological changes or even their absence.
The testicles can be damaged by various influences such as inflammation, tumors, accidents, radiation, surgery or medication. Sometimes they are even absent from birth. For example, an infection with mumps can destroy the testicles in such a way that hormone formation is no longer possible. Sometimes a genetic disorder, such as Klinefelter syndrome, also leads to hypogonadism. In Klinefelter syndrome there is one X chromosome too many. Secondary hypogonadism is caused by diseases in the hypothalamus or pituitary gland.
If the production of the hormones LH, FSH or GnRH is disturbed, the Leydig cells can no longer be sufficiently stimulated to synthesize testosterone. The symptoms of testosterone deficiency depend on the age at which the hypogonadism occurs.If it already exists in childhood or adolescence, the development of the male sexual characteristics is very delayed or not at all. If the testosterone deficiency only sets in in later years, very unspecific symptoms occur in addition to impotence. Since the efficiency of the Leydig cells decreases in the course of life, hypogonadism is typical in old age.
Typical & common testicular diseases
- Testicular cancer
- Undescended testicle (Maldescensus testis)
- Testicular pain
- Epididymitis


.jpg)

.jpg)





.jpg)

.jpg)