The Lipoprotein lipase (LPL) belongs to the lipases and plays a crucial role in lipid metabolism. It is responsible for splitting the triglycerides in the chylomicrons and the Very Low Density Lipoproteins (VLDL) into fatty acids and monoacylglycerine. The released fatty acids are used to generate energy or to build up body fat.
What is lipoprotein lipase?
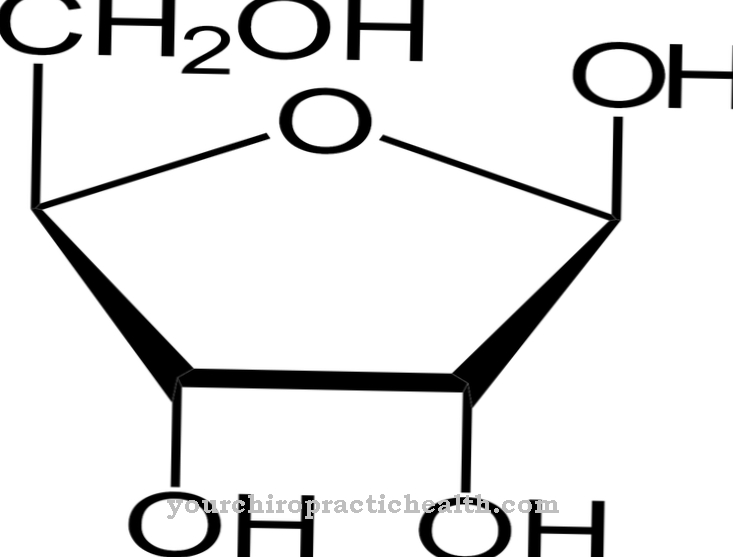
Lipoprotein lipase (LPL) is an enzyme that is one of the lipases. Lipases are responsible for breaking down triglycerides (triacylglycerols) into fatty acids and glycerine. Triglycerides are esters of the triple alcohol glycerine with three fatty acids each. They are known as fats or fatty oils.
Dietary fats are absorbed with food and are first broken down by the extracellular lipases from the pancreas in the intestine. However, some triglycerides get into the bloodstream through the serum when they are absorbed in the small intestine, where they are bound to lipoproteins, which guarantee their transport ability in the blood. The lipoprotein lipase is the enzyme that breaks down the triglycerides bound to the lipoproteins into fatty acids and monoacylglycerol. It consists of 448 amino acids and is dependent on the coenzyme apolipoprotein C2 for its function.
Lipoprotein lipase is a water-soluble enzyme which is bound to the endothelial cells of the blood vessels via certain glycoproteins (proteoglycans). It is produced in the liver. The enzyme catalyzes the hydrolysis of the triglycerides to form two fatty acid molecules and one monoacylglycerol molecule. The apolipoproteins are the carrier molecules of the triglycerins and enable them to be transported in an aqueous environment. Apolipoprotein C2 also acts as a receptor for lipoprotein lipase and thus activates the hydrolysis of the triglycerides.
Function, effect & tasks
The function of lipoprotein lipase is to completely catalyze the breakdown in the blood of the fats absorbed by the intestinal cells. First, the dietary fats are broken down into fatty acids and glycerine by pancreatic lipases in the small intestine. Further triglycerides get into the blood through absorption via the small intestine and there bind to lipoproteins to form a lipid-protein complex.
This creates chylomicrons. They represent lipoprotein particles with a diameter of 0.5 to 1 micrometer. Their density is less than 1000 g / ml. The lipid core mainly contains triglycerides with a small amount of cholesterol esters. The cholesterol-containing shell of the chylomicrons contains phospholipids as a structural element. The apolipoproteins to which the triglycerides are bound are now also stored in this shell. The chylomicrons contain 90 percent triglycerides. They get into the bloodstream from the small intestine via the lymphatic system. The triglycerides are broken down into fatty acids and glycerine with the help of the LPL, especially in the capillaries of muscle and adipose tissue.
The fatty acids are used either in muscle tissue to generate energy or in fat tissue to build up endogenous triglycerides as storage fat. After about ten hours of food abstinence, no more chylomicrons can be detected in the blood because the triglycerides are then completely broken down. Other components of the blood are the so-called VLDL (very low density lipoprotein). These structural units are released from the liver and contain triglycerides, phospholipids and cholesterol. The VLDL transport these components through the bloodstream from the liver to the individual organs.
In this way, the triglycerides are broken down by the lipoprotein lipase and the released fatty acids are absorbed by the body cells. The decrease in triglycerides converts the VLDL into LDL (Low Density Lipoprotein). The LDL mainly contain phospholipids, cholesterol esters and lipoproteins
Education, occurrence, properties & optimal values
Lipoprotein lipase is synthesized in the liver. In addition to the pancreatic lipases, it represents another extracellular lipase. The LPL is located on the outside of the membranes of endothelial cells of various organs, including fat cells. There it is connected to the cell membranes via so-called proteoglycans.
However, it is of particular importance for the endothelial cells of the blood vessels, since here it can directly control the hydrolysis of the triglycerides in the chylomicrons and VLDLs. Heparin is injected to measure lipoprotease activity. Heparin ensures the release of the binding of the lipoprotein lipases from the proteoglycans, so that after a heparin injection there is an increased concentration of free lipoprotein lipases, which can thus be determined via their activity. This examination can, among other things, determine a deficiency in lipoprotein lipase.
Diseases & Disorders
The lack of lipoprotein lipase often leads to serious health problems. If there is too little lipoprotein lipase or if its activity is insufficient due to a genetic defect, the triglycerides in the chylomicrons and the VLDLs can only be broken down poorly or not at all.
The lipoprotein lipase deficiency can be primarily genetic, as well as secondary to chemotherapy, for example. Primary LPL deficiency is rare and is caused by an autosomal recessive genetic defect. A so-called chylomicronemia develops, which is characterized by a milky, creamy serum and is referred to as type I hyperlipidemia. The triglycerides in the chylomicrons are no longer broken down. As a result, severe pancreatides with milk intolerance and abdominal pain occur again and again.
In addition, bursting xanthomas and hepatomegaly develop constantly. The only treatment options are a low-fat diet and no alcohol. This disease is often caused by mutations in the LPL gene on chromosome 8 or in the APOC2 gene. The secondary form of type I hyperlipidemia usually occurs with chemotherapy and is only of a temporary nature.




.jpg)




















