A Lymphangioma is a benign vascular malformation. It is a tumor disease of the lymph vessels that occurs rather rarely.
What is a lymphangioma?

© sakurra - stock.adobe.com
The Lymphangiomas owe their name to their place of origin, the lymphatic vessels. The opposite of the vascular malformations in the blood system are the so-called hemangiomas. Lymphangiomas are divided into three different classes:
- Cavernous lymphangiomas (Lymphangioma cavernosum) usually appear on the face, under the armpits, arms or legs.
- The capillary lymphangioma (Lymphangioma circumscriptum) is found mainly in the skin and mucous membrane area of the mouth and lips. This form can also appear in the genital area or in the groin area.
- If there is a vascular malformation in one or more areas of the neck, throat, armpits, or median membrane, the most likely cause is cystic lymphangioma. These are also called Lymphangioma cysticum or as Hygroma cysticum colli designated.
Occasionally, a fourth form is also described in the medical literature. This lymphangiomatous gigantism is similar in appearance to elephantiasis, an abnormal enlargement of a part of the body caused by lymphatic congestion.
causes
The exact origin of the lymphangiomas is still unclear. The vascular malformations are probably based on an inherited malformation of the lymphatic system. The foundations for the later illness are probably laid in the second month of pregnancy. In the mesoderm, the middle layer of germs, the affected patients then suffer from incorrect differentiation. The lymphangiomas appear to arise from bulges in the venous and lymphatic systems.
The jugular vein, the two pelvic veins and the mesenteric vein in the lower abdomen are particularly affected. Connections are usually established between the lymphatic and venous systems to allow lymph to drain into the veins. In patients with lymphangiomas, however, these connections are partly missing. As a result, the lymph cannot drain and the lymphatic vessels expand.
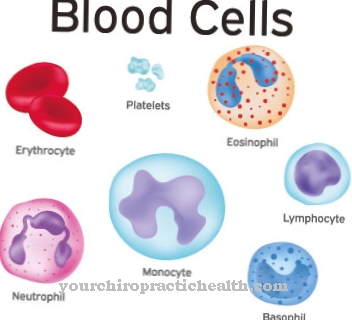
This is also known as lymphangiectasia. The tumor that then forms in these enlargements consists of various cyst-like tissue structures. These are filled with a protein-like liquid that contains many eosinophilic granulocytes.
Symptoms, ailments & signs
The lymphangioma usually appears for the first time in early childhood. In almost 90 percent of all cases, the vascular malformations show up immediately after birth, but at the latest by the age of five.
In most cases the tumor is found on the neck or neck. In 20 percent of the cases, he sits under the armpits. Other parts of the body are rarely affected. The benign tumors can also occur in the mediastinum, on the pleura, on the pericardium, on the vulva, on the penis, in the groin region, in the bones, on the pancreas, on the ovaries or in the entire rest of the abdomen.
In most cases, lymphangiomas are brightly colored or skin-colored. However, bleeding is often found in the cavernous lymphangioma. In these areas the lymphangioma then becomes darker and appears bluish to purple. While the capillary lymphangioma tends to show up in the form of small vesicles, the cystic hygroma and especially the lymphangiomatous gigantism can cause larger tumors.
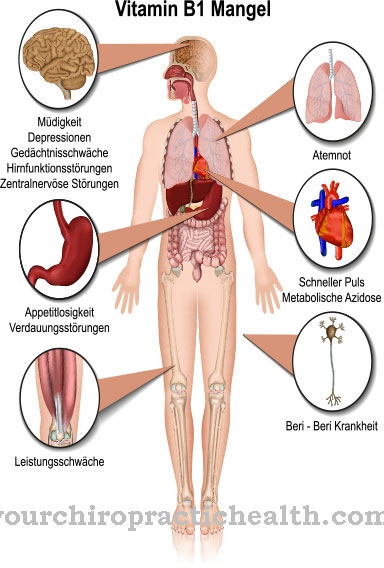
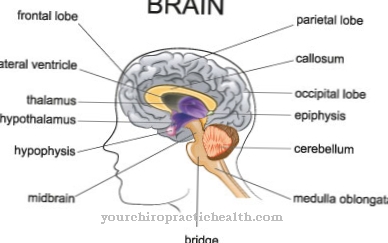
Depending on the size and location, the vascular malformations can also displace other organs and cause corresponding displacement symptoms. A narrowing of the airways can lead to breathing disorders, swallowing difficulties or a forced posture of the head.
Diagnosis & course of disease
At the beginning of the diagnosis there is always a careful examination of the medical history. This part of the diagnosis is also known as the anamnesis. The physical exam follows. In order to be able to differentiate the lymphangioma reliably from other anomalies of the vessels, an ultrasound examination (sonography) must be carried out. The ultrasound also checks whether the position of the lymphangioma has narrowed or obstructed other organ or tissue structures. Magnetic resonance imaging (MRI) may be required for internal lymphangiomas.
Complications
The lymphangioma results in very serious malformations in the patient, which occur primarily in the blood vessels and can significantly limit the everyday life and quality of life of the person affected. In many cases, those affected suffer from bleeding and thus from discoloration of the skin. Furthermore, tumors and growths also develop, which in a very unfavorable case can also spread to other regions of the body.
The malformations in the vessels can have a negative effect on the organs and possibly displace them. This can lead to breathing disorders or difficulty swallowing. Difficulty swallowing often causes difficulties in taking food or liquids. In the worst case, the breathing difficulties can also lead to a loss of consciousness.
It is not uncommon for the lymphangioma to lead to a poor posture of the head, resulting in tension or other unpleasant complaints. Treatment of lymphangioma is done by removing the tumor. Furthermore, those affected are dependent on various therapies even after removal. However, a positive course of the disease cannot always be guaranteed.
When should you go to the doctor?
Lymphangiomas must be diagnosed and treated promptly. Otherwise, the growths can lead to malformations, chronic pain, and other complications. Parents who discover a swelling or lump in their child should inform the pediatrician. General symptoms such as fever, loss of appetite or breathing problems can also indicate a vascular malformation and should be examined. Lymphangiomas are usually unproblematic as long as they are recognized and treated early on. Sick children must be examined regularly even after the deformity has been removed, as there is an increased risk of recurrence.
If a parent suffers from malformations of the lymphatic system, the child should be routinely examined. Since it is a hereditary disease, a specific diagnosis is possible, often while still in the womb. Lymphangiomas are diagnosed and treated by an internist or lymphologist. The family doctor can make an initial suspected diagnosis. If the growth is in the area of the head, the spine or on the limbs, the patient must also be treated with physiotherapy in order to maintain or restore essential body functions.
Therapy & Treatment
In contrast to hemangiomas, lymphangiomas generally do not resolve spontaneously. In most cases, the vascular tumors are completely removed. This complete removal of the tumor is also known as extirpation. For complete healing, the tumor really has to be completely removed. Otherwise there will always be relapses. However, only about a third of all lymphangiomas can be completely removed during the first operation.
Often, tiny vesicles remain along the nerves or organs. They then later fill up with fluid again and form a new lymphangioma. As an alternative or in combination with surgery, laser therapy is often used. The advantage of treatment with the laser is that the procedure is not as stressful as an operation and only small scars remain. However, several treatments are usually necessary for complete removal.
Drug therapies are usually unsuccessful. Only sclerotherapy with picibanil is suitable for drug treatment. A specially treated bacterial strain (Streptococcus pyogenes) is repeatedly injected into the lymphangioma. The procedure is used when the risk of an operation is too great. If organs are affected by the lymphangioma, it may also be necessary to insert a nasogastric tube or a tracheostomy.
In principle, the prognosis of the lymphangioma is to be rated as good. It is a benign tumor, so complete removal means complete cure. The mortality rate is around three percent.
You can find your medication here
➔ Medicines against swelling of the lymph nodesOutlook & forecast
The extent of the malformation is ultimately decisive for the prognosis of a lymphangioma. A good prognosis is made for a large number of patients, since the available options for therapy are often sufficient with current scenic knowledge. In the case of slight changes in the vessels, there may be lifelong freedom from symptoms. In these cases, the diagnosis is often only made possible by a chance finding. However, no spontaneous healing of the disease is to be expected, as the malformations remain lifelong. There is no treatment option that leads to a complete recovery and thus to the elimination of the malformations.
Normally, the tissue changes and the vessels must be treated surgically. Tumors develop that have to be removed so that no further complications occur. Laser therapy is often used to minimize scarring. If the interventions proceed without further disturbances, a significant alleviation of the symptoms can be expected. Nevertheless, checks should be carried out at regular intervals throughout the life to check the functioning of the vessels.
In spite of all efforts, lifestyle choices are limited in a lymphangioma. The physical capacity should be adapted to the requirements of the organism and overexertion should be avoided. With this disease, there are always risks for the development of acute situations, which must be minimized.
prevention
Since the exact causes of the lymphangioma are still unclear, the disease cannot be prevented.
Aftercare
The type and duration of aftercare depends on the location and treatment of the lymphangioma. Often no aftercare measures are necessary. If the benign tumor was surgically removed, the healing of the surgical scars should be observed. If there are postoperative complications, intensive follow-up care is necessary.
As a rule, after successful removal, several check-ups are carried out to determine whether there is a recurrence of a lymphangioma. In some parts of the body, such as the chest area, those affected can determine this themselves by regular palpation. However, regular examinations by a doctor are also recommended in these cases.
The exact interval between the checks is determined by the respective specialist. As soon as those affected perceive changes again, they should therefore consult a specialist, regardless of the agreed control intervals. Those affected should be closely monitored in the event of recurring abnormalities.
You can do that yourself
The lymphangioma has not yet been fully researched medically. For this reason, the possibilities of self-help are not sufficiently well known. Direct sunlight should be avoided to protect against further skin irritation. Cosmetic products should also only be selected and used in consultation with a doctor. It is important to ensure that the benign tumors on the face or neck are not unintentionally scratched, as this can lead to inflammation. In addition, if the mucous membranes in the mouth are infected, the consumption of acidic or spicy foods should be avoided.
Patients and relatives can take advantage of an exchange with other affected persons in self-help groups and forums. Everyday tips and information on how to deal with the disease in everyday life are discussed in a trusting atmosphere. This stabilizes the mental state of many of those affected, relieves fears and clears open questions. The latest experiences are discussed with each other in this way and can help to improve general well-being.
Regular massages help to relieve tension. Depending on the location and extent, the patient himself or with the help of relatives can use circular movements to prevent and resolve the muscle problems. A sufficient and continuous supply of heat is also beneficial for the shoulders and neck area.

.jpg)

















.jpg)



