As Macular edema is a collection of fluid in the human eye. The accumulation of fluid, the edema, is located in the area of the yellow spot. This leads to visual disturbances and especially blurred vision.
What is macular edema?

© Henrie - stock.adobe.com
At a Macular edema a swelling of the retina occurs. The tissue swells, especially in the area of the macula. The macula is a small area in the center of the retina. Since most of the photoreceptor cells are located here, the macula is the place of sharpest vision. The light that falls on an object is partially reflected and then enters the eye. The light is bundled through the cornea and the lens. The light falls on the center of the retina, on the macula.
Here are numerous light-sensitive sensory cells, so-called photoreceptors. The sensory cells convert the incoming light signals into electrical signals. These electrical signals are then relayed to the brain via the optic nerve. This then combines the signals from the eye into a finished image.
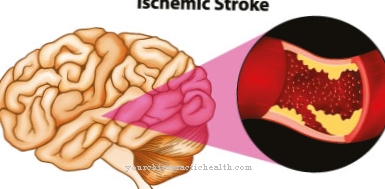
With macular edema, there is a circumscribed swelling and vesicle-like accumulations of water under or in the so-called pigment epithelium of the retina. There are four stages of macular edema. There are focal, clinically significant, diffuse and ischemic macular edema.
causes
There are numerous causes of macular edema. With retinitis or uveitis, swelling of the macula can occur. Retinitis is inflammation of the retina, usually caused by infections with certain bacteria or viruses. Borrelia, Toxoplasma gondii or the cytomegalovirus are possible causes of retinitis.
Retinal inflammation can also occur with certain hereditary diseases. With uveitis, the middle skin of the eye (uvea) is inflamed. Vascular damage to the retina caused by diabetes mellitus is also a frequent cause of macular edema. This is called diabetic retinopathy. Due to the increased sugar level in diabetes mellitus, the small blood vessels in particular, such as the capillaries of the retina, are damaged. This leads to swellings in the area of the retina and thus also to damage to the retina.
This damage often goes unnoticed at first. However, diabetic retinopathy is the leading cause of blindness in Europe. Closure of the retinal veins can also lead to congestion and thus macular edema. Such a retinal vein occlusion occurs when a blood clot (thrombus) forms in the vessel or is washed in from another vessel. The risk factor for developing retinal vein obstruction is arterial high blood pressure. Diabetes mellitus or certain forms of glaucoma also increase the risk of thrombi forming in the blood vessels.
Symptoms, ailments & signs
Macular edema usually develops slowly and remains symptom-free for a long time. With smaller storage, those affected experience problems with the perception of contrasts or colors. In this phase, however, patients can usually still see clearly without any problems. Only with advanced macular edema can there be reduced visual acuity.
Since the point of sharpest vision is affected in macular edema, the visual disturbances also occur preferentially in the central area of the field of vision. Those affected then complain of blurred, blurred or distorted vision. A change in color perception can also occur. There may also be dark spots or red haze in the field of vision. Some patients also report a kind of gray curtain in their field of vision.
Even with the first noticeable signs, there is a risk that the disease will progress to blindness. The symptoms interfere with many activities of daily living. This can lead to problems reading, watching TV or driving a car.
Diagnosis & course of disease
At the beginning of the diagnosis there is always a detailed anamnesis with the ophthalmologist. The existing complaints and the time course of the disease are discussed here. Pre-existing conditions, such as high blood pressure or diabetes mellitus, are also asked by the doctor. Using various examination techniques, the doctor is able to perceive pathological changes in the eye and thus make a diagnosis.
With simple eye tests, the ophthalmologist can also examine visual acuity and contrast and color perception. With a special ophthalmoscope, he can also look closely at the fundus and thus also the patient's retina. With macular edema, typical deposits, vascular changes or even bleeding are visible here. Such an ophthalmoscopy is also known as a fundoscopy or ophthalmoscopy and is part of every detailed examination by the ophthalmologist.
In addition to the funduscopy, so-called fluorescence angiography is often performed. The retinal vessels are made visible with the help of a special dye and a special camera. With optical coherence tomography, the ophthalmologist can also display the individual layers of the retina. In this way, liquid deposits can be detected at an early stage.
Complications
Macular edema usually causes discomfort to the eyes. Visual disturbances develop and those affected can usually no longer see clearly. Furthermore, double vision or blurred vision can also occur. The quality of life of the patient is significantly restricted and reduced by the macular edema.
It is not uncommon for sudden visual problems to lead to depression or other psychological impairments. Furthermore, the disease can negatively affect the perception of colors. Spots appear in the field of vision that can complicate everyday life. Especially in children, macular edema can significantly restrict and delay development. The macular edema restricts the person concerned in his everyday life in many activities and also in work.
Treatment for this disease is usually based on the underlying disease. There are no particular complications. Various medications or surgical interventions can alleviate or completely resolve the symptoms. The life expectancy of the patient is not limited or reduced by the macular edema. In severe cases, treatment with a laser can also be performed. Even with this, there are usually no particular complications.
When should you go to the doctor?
If there are changes in vision, it is advisable to consult a doctor. If you have impaired vision, blurred vision or blurred contours in the field of vision, you should consult a doctor. Special medical tests are necessary so that the cause of the disorders can be determined. If there are changes in color perception, there is also a need for action. As soon as the person concerned notices in everyday life that his color definition differs from that of his fellow human beings, a visit to the doctor is recommended. In these cases there is no spontaneous healing and non-treatment can result in blindness.
If you have a headache, a feeling of pressure in the eye or inside the head, or if you are irritated, a doctor's visit is necessary. If the person concerned suffers from faster fatigue when looking, he needs more strength of the eye muscles to adjust the visual acuity or if there are more accidents in everyday life due to the restricted vision, a doctor must be consulted. Spots or shadows in the field of view are another indication of an existing irregularity. If a veil is perceived in the field of vision, a doctor's visit is necessary so that there is no deterioration in vision. If other people notice an increased clumsiness of the person affected, they should speak to him about it and point out the need for a doctor's visit.
Therapy & Treatment
In principle, the underlying disease must be treated for treatment of macular edema. An optimization of the metabolism in diabetes mellitus or a reduction in blood pressure in the case of increased blood pressure can stop the course of the disease. Various active ingredients for the further treatment of macular edema are currently still being researched. An agent based on a so-called bisindolyl maleimide appears to be promising. In the case of focal macular edema, laser photocoagulation can also be used to prevent further deterioration in vision.
You can find your medication here
➔ Medicines for visual disturbances and eye complaintsOutlook & forecast
The prognosis for macular edema is usually favorable. As soon as the causal disorder has been identified, medical therapy takes place. Without treatment, an increase in symptoms and health impairments can be expected. If the outcome is unfavorable, the quality of life is significantly reduced due to the impairment of vision. The risk of accidents increases and everyday obligations can no longer be fully met. As soon as the person concerned consults a doctor, various medical tests are used to determine the cause of the edema.
There are different treatment approaches that can be used according to individual requirements. In addition to the administration of medication, surgery can also be used. Although this is associated with risks, it is still a routine process that usually runs smoothly. Seldom do complications or other adversities occur that delay the healing process.
Under optimal conditions, the patient can be discharged from treatment as symptom-free within a few weeks. The eyesight is restored. Nevertheless, the patient should take part in regular check-ups in the further course to prevent the symptoms from recurring. Patients diagnosed with diabetes in particular are well advised to have a positive prognosis if they take part in follow-up examinations at regular intervals.
prevention
Diabetics can prevent macular edema with a well-controlled blood sugar level. In addition, regular visits to the ophthalmologist for diabetics are mandatory. But all other people should also have their eyes checked regularly and consult an ophthalmologist immediately if they have visual disturbances.
Aftercare
Since the development of macular edema can often be traced back to an underlying disease, those affected are generally involved in permanent treatment with a doctor in order to prevent further complications or other complaints. An early diagnosis usually has a very positive effect on the further course of the disease. The options for aftercare are largely limited to regular visits to a doctor.
In the event that the eyesight has already been severely affected, follow-up care is aimed at minimizing the visual discomfort. The person concerned should therefore refrain from excessive exertion or stressful activities in which the eyes are over. Are moderately strained, such as hours of computer work and, if necessary, trying to find a visual aid. The correct setting is subject to an expert ophthalmologist.
You can do that yourself
Depending on the cause of the macular edema, an adaptation of the behavior in everyday life and self-help measures to alleviate the symptoms and to prevent a recurrence, a recurrence of macular edema, can help. In many cases the main cause lies in primary or idiopathic arterial high blood pressure as well as in diabetes mellitus type 2. Both underlying diseases promote damage to small and narrow vessels such as the capillaries, so that tissue fluid or even blood can escape.
The adaptation of everyday behavior consists primarily in a careful adjustment of the sugar in the blood and in a consistent lowering of the blood pressure to tolerable values.
In both cases, relaxation techniques are used to support drug therapy, which promote the breakdown of stress hormones and give priority to parasympathetic nerve impulses. For example, conscious breathing exercises, self-hypnosis and Far Eastern relaxation exercises such as Tai-Chi, Qi Gong and yoga are beneficial. The exercises that are carried out regularly serve to set in motion self-repair mechanisms for the damaged vascular system via the parasympathetic nervous system. This reduces the risk of retinal vein occlusion in the area of the macula. Retinal vein occlusions are the main cause of leakage of tissue fluid in the area of sharpest vision.


.jpg)