At Malassezia furfur is a yeast that occurs in the natural flora of almost everyone. The microorganism does not normally damage its host, but can under certain circumstances multiply and then cause inflammatory reactions in the skin, such as reddening and flaking, which in certain cases occur together with itching.
What is Malassezia furfur?
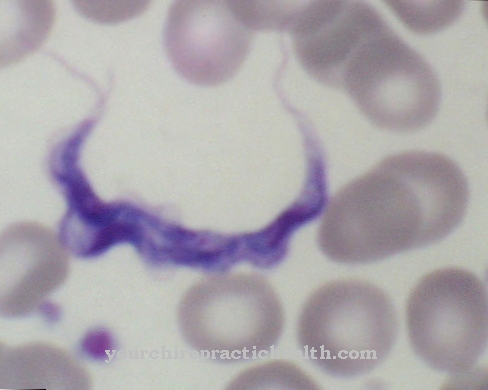
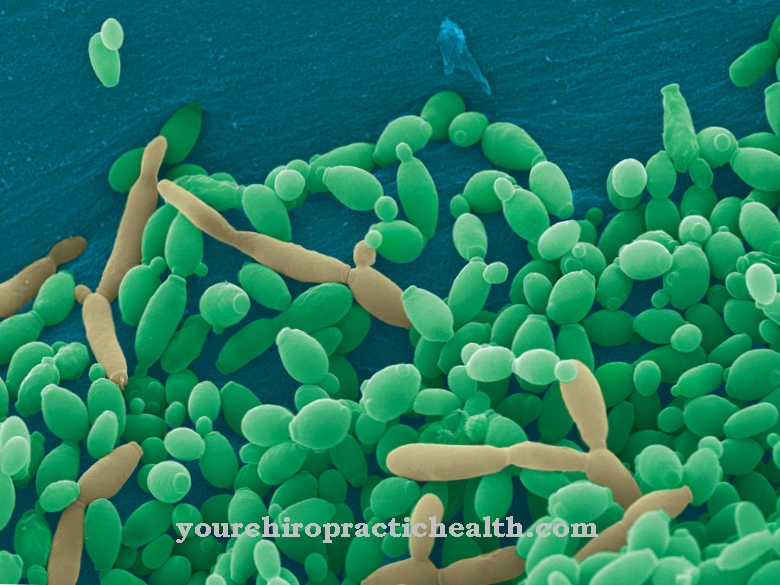
Malassezia furfur belongs to the yeast fungi. These are unicellular fungi that develop energy from the breakdown of organic matter. The fungus is characterized by an oval, cylindrical or round-like cell structure and belongs to the class of Fungi imperfecti. These so-called imperfect fungi are tubular, stand or yoke fungi that multiply through the formation of spores.
The name of Malassezia furfur is composed of Malassezia (after Louis-Charles Malassez, a French medic and bacteriologist from the 19th century) and the Latin term furfur for "skin scab". Malassezia furfur is mainly found in humans, but has also been found in other living things, such as dogs.
Occurrence, Distribution & Properties
The protozoa have a size of 1.5 to 5.5 µm and consist of round or oval fungal cells that multiply through asexual spores. It is believed that the fungus is found in the skin flora of over 90 percent of all people. The transmission and spreading takes place unnoticed. No direct skin contact is necessary for this, just contact with contaminated bath mats, clothing or shoes is sufficient. It can also be passed on from person to animal.
Malassezia furfur has lipophilic properties, which means that it can dissolve fats and oils particularly well. The skin fungus feeds on sebum, which is produced in human skin and consists of long-chain fatty acids. It is therefore particularly common in skin regions where increased sebum is produced, for example on the hairy scalp, on the face or on the chest and back.
Since the onset of puberty is accompanied by increased sebum production, an increased colonization with Malassezia yeasts can be observed for this phase of life. With age, the function of the sebum glands and thus the population density decline again. An extreme increase in fungi and thus skin diseases only occurs in certain and susceptible people, and then repeatedly.
A warm and humid climate is considered to be favorable factors for excessive reproduction. Almost every second person in tropical regions is said to be affected, in the temperate zone only one percent of the population. An immune system that has been weakened by infections or diseases is also a risk factor for excessive Malassezia yeast colonization.
You can find your medication here
➔ Medicines for skin redness and eczemaIllnesses & ailments
If the fungus multiplies too much, it overgrows the other microorganisms of the skin flora. A fungal infection develops that causes scaly, sharply defined spots. Since the fungus can absorb UV radiation, the melanin production of the skin under the fungus is not stimulated, which means that these areas do not turn brown when exposed to sunlight. These skin changes can become increasingly larger and take up entire areas of the skin. A distinction is made between different forms depending on the characteristics.
In pityriasis versicolor, the most common superficial mycosis, the sharply demarcated, yellowish-brown and scaly patches form mainly in the chest and back area. These can spread to the lateral trunk as the infestation progresses. The bran-shaped flaking can easily be wiped off with a wooden spatula. If long-lasting pigment disorders remain after these spots have healed, this is called pityriasis versicolor alba.
Another form of expression is seborrheic dermatitis, which shows itself as whitish-yellowish and greasy skin flakes that occur particularly on the scalp and face. The skin under the scales is reddened due to the inflammation. Often, eyebrows and the beard area are also affected. In most cases, these skin changes in the form of reddening are only perceived by those affected as a cosmetic impairment, as they rarely cause symptoms such as itching or burning.
On the other hand, Malassezia folliculitis, which is characterized by small, extremely itchy papules and pustules, is comparatively rare. Here the fungal infection is no longer just superficial, but the yeast bacteria have penetrated into deeper layers and lead to the aforementioned inflammatory reactions there.
The diagnosis of mycosis can be made by a dermatologist using a so-called radio allergen sorbent test (RAST), in which specific immunoglobulins against allergens are detected in the blood. However, since this examination method takes a comparatively high level of effort, a sample of the scales is usually taken instead by tearing off adhesive tape and examined under the microscope.
Medical treatment is necessary because fungal infections do not heal on their own. For this purpose, the doctor prescribes antimycotics in the form of ointments, gels, shampoos or creams. Fungal infections are persistent, so stopping therapy too early is not recommended. It is also important to ensure that contaminated clothing is thoroughly disinfected to prevent re-infection.
Fungal skin diseases are usually harmless. In exceptional cases there is a risk of systemic mycosis. Here the fungus no longer only colonizes the skin, but reaches the organs via the bloodstream. This is a serious illness that can be very dangerous, especially for people with weakened immune systems, and in the worst case can lead to death.



.jpg)













.jpg)