From one Methemoglobinemia one speaks of an increased proportion of methaemoglobin in the blood. Methemoglobin is a derivative of hemoglobin, which gives red blood cells their color and binds oxygen for transport through the body. Since methaemoglobin cannot bind oxygen, methaemoglobinemia leads to a systemic undersupply of oxygen, which can lead to a. noticeable through bluish discoloration of the skin, tiredness and dizziness.
What is methemoglobinemia?

© jeepbabes - stock.adobe.com
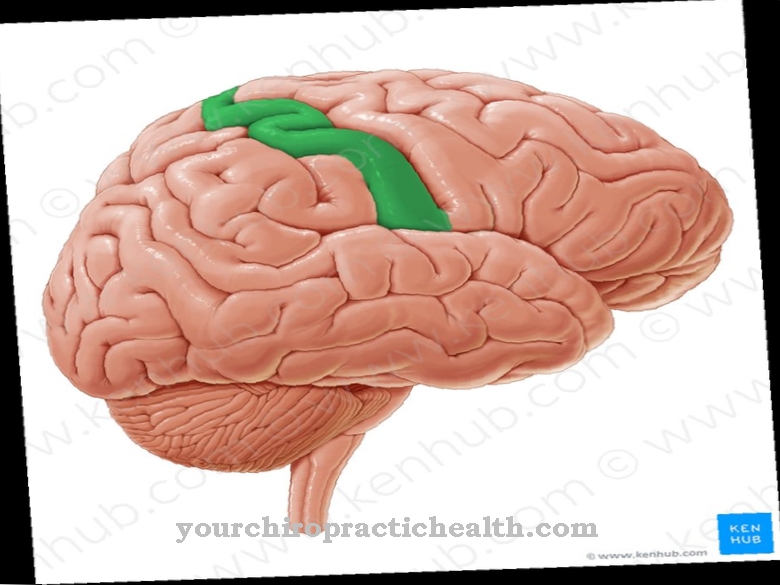
A Methemoglobinemia occurs when the proportion of methemoglobin in the total hemoglobin content of the blood exceeds its physiological value. A precise threshold value is not defined. In a healthy person, the methemoglobin percentage is around 3%. The first clinical symptoms appear from around 10%, serious tissue hypoxia from 30% (especially in the brain).
From 40% methemoglobin content there is danger to life. Hemoglobin (Hb) is a protein that consists of 4 subunits. An iron atom of oxidation level II is embedded in each subunit, which can bind and release oxygen molecules. If the divalent iron atom is oxidized to a trivalent iron atom, methemoglobin (MetHb) is formed.
Methemoglobin is not only unable to bind oxygen itself, but also influences the hemoglobin in its environment in such a way that it only binds the oxygen but no longer releases it. Methaemoglobinemia therefore endangers the oxygen supply to the entire organism.
causes
Basically one differentiates an innate Methemoglobinemia acquired methemoglobinemia. The congenital variant is due to genetic defects in the hemoglobin or in enzymes that prevent oxidation of the hemoglobin, but it is very rare.
Methaemoglobinemia is much more common due to intoxication. Many different substances are possible triggers: In everyday clinical practice, methaemoglobinemia occurs most frequently after the administration of certain medications, including Dapsone and local anesthetics of the amide type. Aromatic compounds in dyes (e.g. aniline) and nitrite compounds are also known to be triggers.
Nitrite poisoning can occur, for example, from curing salt, spinach dishes that are not refrigerated or when preparing baby food with water containing nitrates. Increased cases of methaemoglobinemia in infants (so-called infant lavage) in the 1950s and 1960s led to the introduction of nitrate limit values in drinking water in Germany.
Symptoms, ailments & signs
Which symptoms occur in this disease and what severity they have depends on the one hand on the age of the patient. On the other hand, underlying heart or vascular diseases also influence the severity of the symptoms. If the methemoglobin level in the blood remains below three percent, those affected usually have no symptoms at all.
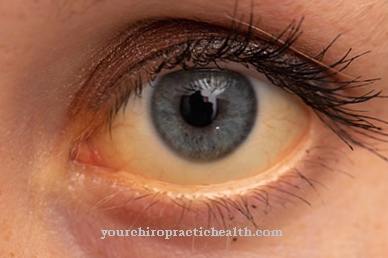
When the three percent is exceeded, the first signs of oxygen deficiency appear. This can be a headache, feeling light-headed or short of breath. In addition, the skin becomes pale and turns greyish in color. If the concentration of MetHB increases to over ten percent, the skin and mucous membranes become bluish (cyanosis) and the arterial blood is clearly insufficiently supplied with oxygen (hypoxemia).
From a proportion of about 30-50 percent MetHB in the blood, one must expect severe breathing disorders, and the vascular functions are also restricted. The blood turns dark and takes on a chocolate-like color. The dizziness increases, there may be brief loss of consciousness and a pronounced feeling of weakness.
If the concentration increases to over 50 percent, the brain can no longer be adequately supplied with oxygen and neurological disorders appear. The patient falls into deep unconsciousness, the heart reacts with rhythm disturbances. From 70 percent MetHB in the blood, there is a high probability of death.
Diagnosis & course
First sign of a Methemoglobinemia is cyanosis, i. H. a bluish to grayish discoloration of the skin. This is particularly noticeable on the lips and mucous membranes.
The methemoglobin itself is brown in color; therefore, under methaemoglobinemia, freshly drawn blood looks chocolate brown. Other symptoms are dizziness, tiredness, impaired consciousness, shortness of breath and an accelerated heartbeat (tachycardia). The diagnosis of methaemoglobinaemia is confirmed by a spectroscopic blood test.
There is also a simple bedside test, in which a drop of normal blood and a drop of patient blood are placed next to each other on a filter paper and compared one minute later. With methemoglobinemia, the patient's blood retains its characteristic brown color. A pulse oximetry measurement of oxygen saturation can be misleading:
This shows a high level of oxygen saturation even with severe methaemoglobinemia. Untreated methaemoglobinemia can be fatal if the oxygen starvation is so severe and persistent that tissue dies. The brain and kidneys are particularly sensitive.
Complications
Methaemoglobinaemia primarily results in a greatly reduced supply of oxygen in the patient. This undersupply has a very negative effect on the overall health of the patient and can significantly reduce the quality of life. In most cases the internal organs are also damaged by this undersupply.
Those affected also suffer from headaches and tiredness, although in severe cases methaemoglobinemia can lead to shortness of breath. The brain is also damaged by the lack of supply. As the disease progresses, there is a loss of consciousness and thus possibly an injury if a fall occurs.
They suffer from impaired consciousness and blue skin. The resilience of the person concerned is significantly reduced by the methaemoglobinemia, so that the performance of ordinary activities or professions can be restricted. As a rule, methaemoglobinemia can be treated relatively easily and quickly, so that in most cases there are no complications or consequential damage.
Complications usually arise when treatment is not given and the undersupply persists over a long period of time. Therefore, methaemoglobinemia usually does not reduce life expectancy.
When should you go to the doctor?
If the person concerned suffers from diffuse complaints that trigger a general malaise or a feeling of illness, a doctor should be consulted. If the symptoms increase gradually over several months, a doctor will need to clarify the cause. Discoloration of the skin, blue lips or shortness of breath are signs of an existing irregularity that needs to be examined and treated. If you experience repeated headaches, dizziness or tiredness, a doctor is advised. A decrease in performance, fatigue or rapid fatigue when performing everyday tasks indicate a health impairment.
A doctor should be consulted so that a comprehensive examination can take place. If there is a disturbance of consciousness, there is cause for concern. In the event of a loss of consciousness, an emergency doctor must be alerted. If left untreated, methemoglobinemia can lead to premature death.
For this reason, medical checks should be carried out in good time in the event of disturbances in the heart rhythm, an increased pulse or a feeling of lack of oxygen in the organism. In the case of sleep disorders, general functional disorders or a loss of well-being, a doctor is required.
Treatment & Therapy
The prognosis of a Methemoglobinemia is usually good. Slight intoxications recede on their own if the toxic substance is no longer administered.
This regression is based on the fact that erythrocytes are constantly broken down and newly formed in the human body (around two million per second) and the poisoned erythrocytes are exchanged in this way. In the case of serious poisoning, therapy consists of the administration of oxygen and the intravenous administration of solutions with redox dyes such as methylene blue or toluidine blue.
In very severe cases, a blood transfusion may also be necessary. Another antidote is ascorbic acid (vitamin C). Daily vitamin C doses are the drug of choice for hereditary methaemoglobinemia; these are not curable, but can only be alleviated.
You can find your medication here
➔ Medicines against impaired consciousness and memory problemsOutlook & forecast
The prognosis for methaemoglobinemia is usually favorable. Not all patients need medical care. In some cases, healing occurs spontaneously, so there is no need for further action. If the illness can be traced back to the administration of medication, a change in the prescribed preparations can already contribute to a recovery of the methaemoglobinemia.
However, if there is a genetic disease, the person concerned will need drug treatment in the course of life so that their situation can improve. The therapy helps to optimize the proportion of methemoglobin in the blood and to meet the needs of the organism. The patient must expect to take part in long-term therapy that otherwise the symptoms will return within a few weeks or months.
Without making use of medical care, the quality of life of those affected with a genetic disease is restricted over the entire life span. In these cases the prognosis is worsened due to the discomfort. In acute phases or in the event of severe disease, ultimately only a blood transfusion can alleviate the symptoms. Here, too, it is possible that this measure will have to be used several times in the course of a person's life, as it is only a temporary improvement in health.
prevention
One Methemoglobinemia can essentially be prevented by avoiding dealing with toxic triggers. Infants who are particularly susceptible to methemoglobinemia should not consume foods high in nitrite.
Aftercare
Follow-up care for methaemoglobinemia is similar to preventive measures. So it is primarily about the treatment of the causative disease. To minimize the risk in children, parents should take care that breathing is not restricted by mechanical influences.
In general, follow-up care is based on whether the disease is congenital and whether it is caused by poisoning. Adults over 35 years of age are advised to attend a regular check-up. These tests can be used to detect changes and abnormalities at an early stage so that rapid therapy can be initiated.
You can do that yourself
In methaemoglobinemia, it is usually sufficient to avoid the triggering substance. Patients who take medication regularly should switch to another medication or reduce the dose in consultation with their doctor. If the typical symptoms arise as a result of excessive ingestion of curing salt or spinach dishes, a doctor's visit is also indicated.
Those affected should also change their diet and speak to a nutritionist if their symptoms persist. The individual symptoms must be treated individually. Sleep and gentle sedatives and painkillers from naturopathy help with headaches and tiredness. Dizziness and confusion can usually be relieved by exercise in the fresh air. Depending on the intensity of the symptoms, bed rest and rest is also indicated.
If complications arise, methaemoglobinemia must definitely be hospitalized. Eating adequate diet and drinking plenty of fluids is important before treatment for methaemoglobinemia. Otherwise, circulatory shock and symptoms such as fever can occur. After the therapy, the patient should first go to bed and rest. The doctor responsible can give further tips on how the symptoms can best be overcome.

.jpg)


.jpg)