If a breastfeeding mother's breasts harden in the first few weeks or as the breastfeeding continues, then a Milk congestion exist. This shows up in a hardened, hot and painful chest. In addition, complaints such as fatigue, headache and body aches or fever can be added.
What is milk congestion?

© SENTELLO - stock.adobe.com
If the breast is not completely emptied while breastfeeding, milk will remain. This cannot drain, which creates a blockage in the milk ducts. Such a blockage is uncomfortable and can also cause pain. Most of the time, milk congestion occurs at the beginning of the breastfeeding period, when the mother's breast produces a lot of milk due to the leakage of milk.
This can usually not be completely drunk by the infant. But even after a few months, milk congestion can still occur. It is often enough if the baby only overslepts one meal and the breasts begin to tighten. Hardened areas can then also be felt, which feel like a small warm lump. A milk congestion should not be confused with the preliminary stage to mastitis (breast inflammation), in which the tissue around the milk duct is swollen and thus presses on it and prevents the milk flow.
causes
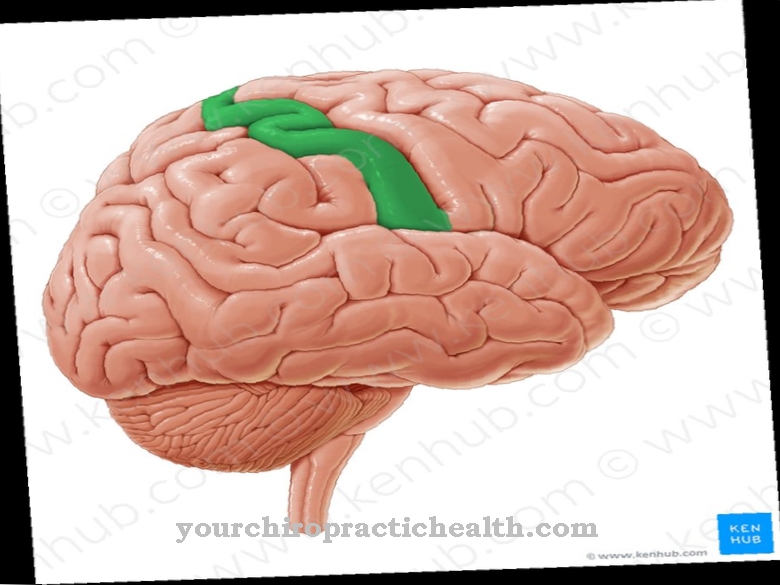
Several glandular lobes make up the mammary gland. These glandular lobes consist of milk-forming vesicles and a network of milk ducts. The milk flows from here to the nipple. A milk blockage occurs when these milk ducts are blocked and therefore not completely emptied. There is an increase in pressure in the milk ducts, which is associated with tension and pain.
The causes for such a blockage are very diverse. First of all, a lack of milk ejection reflex can lead to milk congestion. Normally, the mother's body releases the hormone oxytocin. As soon as the child sucks on the breast, the milk flows. However, physical exertion or stress or exhaustion can impair the milk delivery reflex and the milk can build up.
Furthermore, excessive milk production can also be the cause. This produces more milk than the baby actually needs. An imbalance usually arises when an infant suddenly falls asleep and no longer needs a nightly meal or a milk meal is replaced with porridge. So the amount of milk increases while the amount you drink decreases. Normally this regulates itself quickly.
The most classic cause of a milk congestion are usually mechanical disabilities. The reasons for this are incorrect application or incorrect suction as well as short and infrequent breastfeeding meals. The breast cannot be completely emptied this way. Sometimes a bra that is too small or clothing that is too tight can block the flow of milk.
In addition, some women are more prone to breastfeeding problems, which then increases the risk of milk congestion. This is the case, for example, with mothers of multiple births or with women who have previously had breast surgery.
Symptoms, ailments & signs
Milk congestion occurs in many mothers while breastfeeding. In most cases, this is the case shortly after the birth, the breastfeeding relationship is still very fresh and the baby has not yet found the optimal sucking technique. The milk ducts are therefore not completely emptied.
Classic signs of a blocked breast are local chest pain, induration and small palpable nodules in the breast or small and white blisters on the nipple. The chest is also excessively plump and warm to hot, and the nipples are very sensitive to touch. The skin on the chest may also be reddened and the temperature slightly increased, but general well-being is not impaired.
Complications
If the blocked milk remains untreated and the breast is still not completely emptied, a breast infection can result. Germs that multiply in pent-up breast milk are usually responsible for this. But even without germs, an infection can develop in the milk ducts. This happens when breast milk gets into the tissues around the breast, causing inflammation. A breast infection caused by bacteria (e.g. Staphylococcus aureus) is accompanied by a fever of up to 40 degrees Celsius and causes flu-like symptoms.
Sore nipples can occur if the milk becomes blocked. Through the sore nipples, in turn, due to stronger suction, germs from the mouth and throat of the baby can get through the sore spots into the breast, where the nipples then become inflamed.
One problem with breast inflammation resulting from a blocked milk is that the milk has a different taste and it can happen that the infant stops drinking or refuses to breastfeed after just a few puffs. To avoid further pain, the breast should then be emptied by pumping.
When should you go to the doctor?
If the pain becomes stronger with a blocked milk or if there is still no improvement after two days and the affected areas are swollen, warm and reddened, the breastfeeding mother should see a doctor. This is especially important if there is a deterioration in the general condition, headache and body aches, fever and chills. In this case, the blocked milk has already developed into breast inflammation.Therefore, in the event of complaints: Better to see a doctor too much to avoid such mastitis.
diagnosis
Milk congestion can usually be diagnosed quite easily on the basis of a detailed anamnesis and a physical examination. As part of the anamnesis, questions are asked about the complaints. During the physical examination, the affected breast is palpated very carefully in order to cause the patient as little pain as possible.
The doctor will also ask about possible psychological stress in order to research a possible cause of the blocked milk. During the diagnosis, an additional examination is carried out to determine whether there are any signs of the development of a breast infection. In this context, in the event of symptoms such as fever and chills, a further examination to rule out puerperal fever immediately after delivery makes sense, because this can be life-threatening if treatment is not taken.
Treatment & Therapy
In the treatment of a milk blockage, the "cooperation" of the patient concerned is particularly important. In most cases, conservative treatment measures such as emptying the breast through regular breastfeeding or, if necessary, stroking and pumping, the correct breastfeeding position, warming the breast before and cooling (e.g. with quark compresses or cool pads) after breastfeeding as well as plenty of rest and Relaxation are the most important treatment approaches to treat congestion.
In the past, nasal spray containing oxytocin was often recommended, which is said to be helpful when emptying milk. However, such nasal sprays are no longer approved in Germany due to a lack of information on safety.
In most cases, specific medical treatments are not necessary. However, if mastitis develops from the blocked milk, the doctor will prescribe antibiotics. If milk congestion occurs during or a short time after weaning, weaning tablets are often helpful. In consultation with the doctor or midwife, breastfeeding-friendly painkillers can also be taken if the pain is unbearable.
Alternative treatment methods such as acupuncture, traditional Chinese medicine and the use of medicinal plants and herbs and essential oils can also be useful in the case of milk congestion. Homeopathic remedies such as globules can also be helpful without the milk being exposed to chemical substances.
Outlook & forecast
The prognosis for a milk blockage is very good overall. It is very easy to treat, and affected women have several options to choose from. The best chance of success with blocked milk, however, is pumping, although it should be noted that this in turn promotes milk production. However, it brings the necessary relief to the breast and removes the blocked milk for some time. However, it can recur at any time, for many reasons.
Physical and psychological stress, for example, are considered to be important causes of a milk blockage. Accordingly, there are some women in whose lives congestion is more common than others. Frequent congestion is easy to treat, but carries a certain risk of developing breast or gland infections. Such an inflammation is treatable, but very painful.
In almost all cases, however, emptying the breast will remove it if there is a blocked milk. There are then no consequential damage or possible complications to fear. The breasts are not changed or become ill, even with frequent obstructed milk, if action is taken quickly. It is more important to take preventive measures so that milk congestion occurs less often.
prevention
Milk congestion cannot be completely prevented. However, taking some preventive measures can reduce the risk. Breastfeeding mothers should always wear loose clothing that does not restrict them. Especially after the birth, excess milk that the baby does not yet need should be pumped out or at least spread out until the supply and demand for milk are optimally coordinated.
If too much breast milk is produced or if the milk blockage is already beginning, certain milk-promoting drinks should be avoided. Breastfeeding and herbal teas in particular should then be deleted from the drinks list. Sufficiently long recovery phases are also useful, because stress can also lead to congestion. The household and the care of the child should also be left to the father.
Aftercare
A milk blockage can recur any time after it has healed, which is why it is important to control the milk flow immediately afterwards. Above all, it is crucial to ensure that the chest is emptied as much as possible. If the child has not drunk everything, it can help to spread out the remaining milk in order to avoid a new build-up.
Follow-up care is therefore more focused on preventing breast inflammation. Once invading germs have settled in the pent-up breast milk and caused an infection, further complications can result.
It is important to normalize the changed drinking behavior of the child as quickly as possible. In the event that this does not seem feasible, an alternative is to switch to bottle feeding so that the child does not suffer from dehydration and lack of nutrients.
You can do that yourself
Breastfeeding mothers should consult their midwife or lactation consultant as soon as the first signs of a blocked milk condition appear. They have experience with such problems and can provide good assistance.
Of course, it is also important to continue breastfeeding. Contrary to what is often recommended, breastfeeding should not be reduced or shortened. It is important that the breast is drunk empty, especially for prevention or in the event of a blocked milk. Breastfeeding as needed and when there are early signs of hunger is the motto. Since the problems usually begin with sore nipples, a change of the breastfeeding position can be helpful, because the wrong positioning and breastfeeding technique is often responsible for sore nipples. Furthermore, sufficient hygiene should be ensured.
Since germs can get into the open areas and cracks, especially with sore nipples, regular hand washing before touching the breast is extremely important. In the event of a blocked milk, a warm full bath can also be helpful, because the warmth causes the milk to flow almost by itself after around 30 to 40 minutes. The warm water also has a relaxing effect and helps to stimulate the milk donation reflex.
Warm showers, envelopes or church pillows can also be helpful. Midwives and lactation consultants also like to show expectant mothers certain massage techniques with which the milk can be gently and gently spread out.



.jpg)
.jpg)

.jpg)