A minimal state of consciousness (MCS) should not be confused with a vegetative state, although both diseases are very similar. Affected people appear temporarily awake, as the eyes are open and movements as well as a mine game are present. A minimal state of consciousness can be temporary as well as permanent.
What is a minimal state of consciousness?
.jpg)
© Sebastian Kaulitzki - stock.adobe.com
A minimal state of consciousness (MCS) - also as Minimal Concious State - is a twilight state that is very similar to that of the coma.
In contrast to the vegetative state, however, those affected occasionally react to external stimuli, such as B. touches, sounds or light effects. The minimal state of consciousness is controlled by the autonomic nervous system, which functions independently of the cerebrum, so that there is still a sleep-wake rhythm.
A minimal state of consciousness can develop from a coma or from a vegetative state. It can be temporary, but after about 12 months the likelihood of the person waking up from the minimal state of consciousness decreases and it changes to a permanent state.
causes
There are several causes of one minimal state of consciousness. MCS has a disorder in the cerebral function. This is often triggered as a result of illness or injuries.
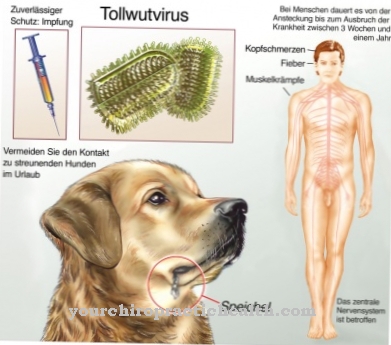
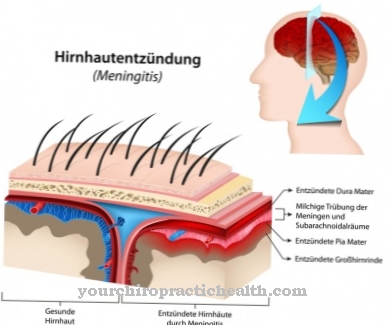
The following diseases or disorders in the brain can lead to a minimal state of consciousness: Apoplexy (stroke), traumatic brain injury, epilepsy, meningitis, encephalitis, tumors, cerebral haemorrhage.
But also metabolic diseases such as B. Diabetes mellitus, liver dysfunction, thyroid disease and kidney disease can be a trigger for the minimal state of consciousness. In addition to cardiovascular diseases, alcohol and drug abuse can also trigger a minimal state of consciousness.
An MCS does not occur immediately. If the above If the causes take a severe course and the patients fall into a coma, a minimal state of consciousness can develop from this.
Symptoms, ailments & signs
The doctor bears a great deal of responsibility in correctly distinguishing between the syndrome of unresponsive wakefulness (SRW or vegetative coma) and the state of minimal awareness (MCS). Misdiagnoses are often the result, with the rate of misdiagnosis being extremely high at around 37 to 43 percent. In the classic vegetative state, there is no evidence of the patient's ability to make contact, although there are phases of wakefulness with open eyes.
With a minimal state of consciousness (MCS), the patients show behaviors that suggest a conscious perception of the environment. While those affected in the syndrome of unresponsive wakefulness show no reactions to external stimuli, people with MCS sometimes react to touch, sounds or visual impressions. Among other things, you can move your hand, foot or another part of the body when prompted.
Some people affected can follow a moving object through eye contact or perform certain agreed gestures in response to questions that must be answered with yes or no. MCS is always preceded by a vegetative state. It is a transitional state between coma and full consciousness. The patient can remain in this state for years or even forever.
However, this condition can also prove to be the baseline for a full recovery. The error rate in the correct delimitation is so high because there are also patients with MCS who can experience the environment consciously, but for various reasons have no opportunities to show reactions.
Diagnosis & course
The diagnosis is made minimal state of consciousness from neurologists. Diagnosis is extremely difficult because MCS and vegetative state are very similar. Imaging techniques are used to diagnose a minimal state of consciousness.
In addition to regular MRI and CT, so-called functional magnetic resonance imaging (fMRI) is also used. In the colloquial area, the fMRI is also referred to as a brain scanner. With the help of this examination method, the brain activities in the different regions of the brain can be measured.
The course at a minimal state of consciousness is not promising. The likelihood that sufferers will wake up from the MCS is higher than waking up from the vegetative state. In the first few weeks and months, it is most likely that the person will wake up. However, if more than 12 months have passed since the start of the MCS, it becomes increasingly unlikely that the affected person will wake up. The minimal state of consciousness becomes a permanent state.
If an affected person wakes up from the MCS, i. d. R. heavy damage back. The longer the MCS has lasted, the more pronounced the physical and mental disabilities will be. A minimal state of consciousness can last for many years before the person ultimately dies.
Complications
The minimal state of consciousness has a very negative effect on the quality of life of the person concerned and can lead to very serious psychological complaints or to depression. Those affected are in a vegetative state and can no longer eat or drink alone. As a rule, you are therefore always dependent on the help of other people.
Furthermore, the eyes are open so that the patients always hear events from the outside world, but cannot actively participate. Even speaking is usually not possible either. Furthermore, there is also an incontinence of the patient. Not infrequently, the parents, children or relatives of those affected are clearly affected by the minimal state of consciousness and suffer from severe psychological limitations and depressive moods.
It cannot generally be predicted whether this will lead to a positive course of the disease or whether the affected person will spend his entire life in this condition. A targeted treatment of the minimal state of consciousness is usually not possible. The joints can be supported with various therapies so that they do not stiffen. In most cases, however, life expectancy itself is not reduced or influenced by this condition.
When should you go to the doctor?
With a minimal state of consciousness, many patients are already under medical treatment. Normally you only need help and support if your health condition deteriorates or if you suddenly notice abnormalities.
If the person concerned notices an impairment of his state of consciousness in everyday life without a diagnosed illness, he should consult a doctor. If the condition has persisted for a long time or if there are further decreases in consciousness, there is cause for concern. Since in some cases there is a serious illness, it is advisable to see a doctor as soon as possible. If members of the social circle notice the minimal awareness, they are asked to get help. Often the sick person is not in the health condition to notice the existing irregularities.
Signs are open eyes of the person concerned and at the same time inability to engage in social interaction appropriate to the situation. If communication with people in the immediate vicinity is not possible, a doctor should be called. Behavioral problems such as apathy, drowsiness, or persistent mental absence must be presented to a doctor.
If urine or stool incontinence occurs, a doctor should be consulted. If the person concerned is unable to control his or her sphincter muscle, he or she needs medical help. If you cannot cope with everyday life independently, a doctor's visit is necessary.
Treatment & Therapy
At the beginning of a minimal state of consciousness intensive medical care takes place. Afterwards, those affected can be transferred to the hospital's nursing departments or to special care facilities. It is also possible for the relatives to take care of the care at home.
In addition to general medical care and professional care, physiotherapy, occupational therapy and speech therapy measures are particularly useful. With the help of physiotherapy and occupational therapy, the various limbs are moved so that the joints do not stiffen. In addition, various stimuli are used to stimulate hearing and vision. There are special music therapies and so-called basal stimulation, in which sensory stimuli are used to try to induce a reaction in the person affected.
Outlook & forecast
The prognosis regarding the emergence of a minimal state of consciousness (MCS) depends on the cause and the respective patient. First of all, it should be noted that a younger age increases the chance of surviving brain injuries and the resulting changes in the state of consciousness. At the same time, the prognosis for non-traumatic brain injuries that led to MCS is worse than for traumatic brain injuries. Ailments affecting the whole or large parts of the brain (infections, tumors, etc.) are therefore worse for the prognosis than severe injury as a result of an accident.
In addition, patients in the minimally conscious state have a significantly better prognosis than those in the vegetative stage. Since the two conditions are not always correctly differentiated, MCS patients are occasionally treated as patients in the vegetative stage. This leads to a worse prognosis because the treatment is mostly purely palliative and does not work towards a possible improvement in the state of consciousness.
In addition, over time it becomes less likely that those affected will grow out of their condition. Most who do grow up within the first three months, while this is extremely unlikely after twelve months.
Permanent damage in the form of restricted brain functions and associated problems remain in almost all people who were in a minimal state of consciousness. Some restrictions can be compensated for with suitable therapies.
prevention
One minimal state of consciousness cannot be prevented. Only general prophylactic measures can be taken, in terms of accident prevention in the home, at work and in traffic.
In addition, eating a healthy diet and getting enough exercise are good measures for a long and healthy life. In order to prevent illnesses or to recognize them in good time, it makes sense to regularly take part in preventive and health examinations. If you really get sick, you have a good starting point to defeat the disease so that a minimal state of consciousness (MCS) cannot develop from it.
Aftercare
Follow-up care plays an extremely important role for those affected who suffer from the minimal state of consciousness. Thus, depending on the extent of their activity restrictions, the patients continue to need care even after their discharge from the hospital. This also applies to regained independence. The rehabilitative aftercare takes place on an outpatient basis and extends over a longer period of time, the duration of which cannot always be determined.
Since those affected can no longer live alone, accommodation in a shared apartment is recommended, where intensive care outside the hospital is provided. However, 24-hour care is also possible in the familiar environment. In mild cases, assisted living can also be carried out. Some of those affected are even able to work in a special workshop for disabled people.
Seriously ill people, on the other hand, need permanent care in a day care center or a practice for outpatient neurorehabilitation. Many patients can still recover from apallic syndrome after years in their familiar surroundings. Consultations are possible through the care insurance.
They have the task of advising those affected individually on care within their own domesticity. Special care support points are also available in numerous regions. Early rehabilitation is an important part of aftercare. It continues acute treatment from the hospital and includes therapeutic care, physiotherapeutic measures, speech and swallowing therapy, occupational therapy and neuropsychological treatments. The aim is to improve the patient's state of consciousness. Whether a full recovery is possible depends on the individual.
You can do that yourself
Patients who are in the minimal state of consciousness can do little for themselves or for the improvement of their situation. The relatives or the nursing staff are therefore primarily responsible for optimizing the framework conditions for the patient.
In particular, hygiene and sleeping conditions are important so as not to cause additional complaints. The patient's body needs to be moved regularly and cleaned thoroughly.Since the sick person is unable to do this himself, helping hands should take over these tasks. The sleeping area must also be cleaned and provided with clean sleeping utensils. It is important to minimize the risk of the development of bacteria or other pathogens, as the patient is very susceptible to other diseases due to his or her health. The supply of fresh air should not be forgotten. This has a beneficial effect on the patient's airways.
Several studies suggest that the closeness and voice of loved ones can have a positive influence on the course of the disease. It is therefore advisable to talk to the patient or read stories to them, even if the patient cannot answer. At the same time, relatives should take care of their own well-being. Psychotherapy or relaxation methods help to strengthen their mental strength when dealing with the disease.