rabies, Rabies or Lyssa is a deadly infectious disease caused by viruses. Most of the time, rabies is transmitted to humans through wild animals such as foxes, martens and bats. Not infrequently, however, also from infected feral cats or dogs. Without vaccination and treatment against rabies, the disease is 100% fatal.
What is rabies?

rabies is an infectious disease that is mostly transmitted by infected animals such as foxes or dogs. However, rabies itself is triggered by so-called rabies viruses. In addition to dogs and foxes, martens, badgers and bats can also transmit rabies to humans in Germany.
Since rabies is systematically combated in Germany, the probability of being infected by an infected animal has decreased significantly in recent years. However, occasional infections do occur. The incubation period of rabies is indicated by research from three to eight weeks. At the same time, the outbreak of the disease also depends on the amount of virus transmitted.
Rabies is notifiable in Germany and should be treated immediately by a doctor, as the disease can be fatal if left untreated. In Germany itself, only up to three cases of rabies occur per year. In India, however, 15,000 and in China around 5,000. Travelers to these countries should therefore think about a rabies vaccination and seek advice from a doctor.
causes
The causes of the rabies can be found in the rabies viruses, which belong to the rhabdo viruses. Transmission or infection with rabies mostly occurs through wound infection such as bites, but also through saliva from infected animals or humans.
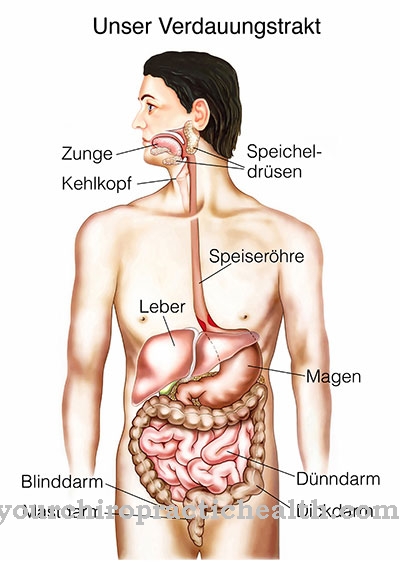
The virus then spreads in the immediately affected muscles of the wound and then continues to multiply via the nerves to the brain.
Here, in turn, they get into the salivary glands, such as the pancreas, where they can be transmitted through saliva, digestive juices and sweat.
Symptoms, ailments & signs
The symptoms of rabies disease can be divided into three stages. In the first stage, the prodromal stage, the signs of rabies disease are unspecific. Patients complain of headache and stomach ache, and a fever develops, which can rise sharply as the disease progresses. Vomiting and diarrhea are other common symptoms.
If the rabies was transmitted through a bite, the wound around the bite site may itch. In the further course, an increased irritability of the patient is observed. Those affected are often sensitive to water, light, drafts and noise. The second stage is called the excitation stage. At this stage, the brain of the affected patient is already affected and the symptoms of the first stage are accompanied by neurological signs of illness.
Patients develop an intense, even panic fear of water, which is also triggered by water noises such as rustling or splashing and swallowing their own saliva. Many patients therefore no longer swallow; the larynx may cramp and saliva may leak from the mouth. In atypical cases, symptoms such as seizures, confusion, aggression and hallucinations appear in the second phase.
In the third stage, the paralysis stage, more and more paralysis occurs in rabies disease, as a result of which the patient falls into a coma. The symptoms of paralysis affect all muscles and affect breathing.
Course of disease
The course of the rabies depends on the early detection of the disease. If the infected person is treated immediately after a bite by an animal infected with rabies, the chances of recovery are good and complications are rather rare.
However, if the brain is infected by the rabies virus and the typical rabies symptoms appear, the disease is no longer curable. Death can no longer be averted and can only be delayed by means of intensive medicine. So far, there has only been one case worldwide in which a patient survived rabies.
Complications
A rabies infection that has already spread to the brain always brings death as a complication. All complications of rabies can usually be avoided by vaccination immediately after possible exposure. The mortality rate for nested rabies is almost 100 percent. It is therefore necessary to visit a doctor or hospital quickly after a bite from an animal that tends to be ill.
For example, after rabies has spread in the body, it can kill the person in several ways. The most common complication leading to death is an incipient coma with respiratory failure. But also a cerebral infarction, meningitis, encephalitis and many other symptoms of the disease lead to death. The other complications are caused by seizures, hydrophobias or photophobias, enormous saliva formation and the other characteristics of inflammation.
The course of an outbreak of rabies is often not properly treated, since paralysis and respiratory depression in particular suggest a disease of Guillain-Barré syndrome. Accordingly, the dying patient is not immediately treated according to his illness (palliative). In addition, if you have Guillain-Barré syndrome, no protection against infection by other people is necessary, which makes the transmission of rabies more likely.
When should you go to the doctor?
Rabies is a serious disease that requires medical attention in any case. A doctor should always be consulted after contact with an animal that may be infected with rabies. Rabies vaccination is also necessary if a suspicious animal has licked the skin. The typical symptoms usually appear three to eight weeks after infection. If you experience unusual physical or psychological complaints during this period, we recommend that you see a doctor. Typical warning signs are headache, gastrointestinal complaints and fever. The painful bite is the clearest indicator of infection.
Emergency medical treatment is required after a bite. Otherwise the fever will continue to rise and cause severe physical discomfort. If the patient vomits his own saliva, the emergency doctor must be alerted. People who frequently come into contact with forest animals are particularly at risk. A precautionary rabies vaccination is recommended before traveling to Africa, Asia or Latin America. Upon return, the general practitioner should be consulted for a routine check-up. The doctor can identify any pathogens with a saliva test and initiate appropriate treatment.
Treatment & Therapy
After a bite from one potentially rabies sick animal, the doctor should treat the disease as soon as possible. In the hospital, the infected wound is cleaned with strong soapy water and water. The aim is to wash out the rabies virus before it can multiply in the muscles. Furthermore, attempts are made to kill the pathogen with the help of alcohol and to disinfect the wound.
If the wounds are already very deep, catheter rinsing may be necessary. These treatment measures are always carried out in the intensive care unit and are strictly monitored. After washing out, a so-called dead vaccine is vaccinated. This vaccine and additionally administered immunoglobin are intended to immunize the patient against rabies. A vaccination against tetanus or tetanus is often carried out as a preventive measure.
prevention
It is best to bend against it rabies with a vaccination. This is not covered by all health insurances, but should be taken into consideration especially by travelers to America and Asia or veterinarians and hunters. The protection of this vaccination then lasts for 5 years.
Other preventive measures include avoiding contact with wild and unusually tame or aggressive wild animals. Wild or conspicuous animals should not be touched or only touched with the help of protective gloves.
Aftercare
After the initial medical treatment of the wound, the bite site must continue to be checked for the next 24 to 48 hours. It is important to identify any possible infections and other complications early on. If necessary, these must be treated. It depends on the individual situation, at what intervals these controls are necessary.
In order not to endanger the healing process, the wound must be observed for adverse changes. Care is taken to see whether the wound is reddening or swelling. Joint pain, restrictions on the range of motion or fever must also be taken seriously. In this case, a doctor or an emergency department should be consulted immediately.
In the worst case, a generalized infection such as blood poisoning or sepsis can develop if there is no timely response. If this remains untreated, death can occur. It is also advisable to have a rabies vaccination after a bite. Here, 20 IU per kilogram of body weight of human rabies hyperimmunoglobulin are administered once by syringe.
There are no contraindications that speak against such a vaccination after being bitten by an animal suspected of rabies. Even if the patient does not go to the doctor until a few weeks or months later after the bite, a post-exposure vaccination must be carried out. It must also be checked whether the patient is protected by an adequate tetanus vaccination. If necessary, this should also be refreshed.
You can do that yourself
In the case of rabies, it is important to act quickly. If symptoms of illness, such as fever and pain, are noticed following an animal bite or contact, a doctor must be consulted immediately.
Immediate vaccination can often prevent the disease from breaking out. Careful cleaning of the wound is also important. By using special rinses, a large part of the viruses can be removed before they enter the body. Prophylaxis can also be useful for relatives of the sick person.
After the active and passive vaccination, rest and rest. The course must be carefully monitored and the active vaccination repeated after three, seven, 14 and 28 days. In addition, immunoglobulin therapy can be carried out.
After treatment, the cause of the possible rabies infection should be determined. After an animal bite, for example, the responsible animal must be caught and examined. However, prophylaxis takes place before the animal is diagnosed in order to improve the chances of recovery. If it turns out that the animal is not sick, the treatment can be stopped.




.jpg)

















.jpg)



