Mitochondrial diseases are diseases of the mitochondria. These are located in almost every cell in the body and supply the body with energy. The characteristics and symptoms of mitochondrial disease can be very different.
What is Mitochondrial Disease?

© vecton - stock.adobe.com
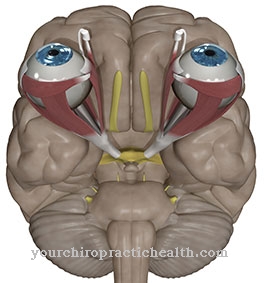
Mitochondria are small cell organelles. Important metabolic processes take place in them. As part of the respiratory chain, for example, energy is obtained in the form of adenosine triphosphate (ATP). At a Mitochondrial disease there is a disturbance in the proteins of the cell organelles. This means that not so much energy can be obtained. The brain and eyes in particular are affected by mitochondrial disease. The disease can be acquired or congenital. However, there are also flowing transitions between the two forms.
causes
Mitochondrial disease is caused by damage to or malfunction of the mitochondria. Hereditary mitochondrial disease is caused by gene mutations. These affect the enzymes and metabolism of the mitochondrion. The genetic defects are already present at birth. Mutations in mitochondrial DNA are only inherited from the mother. However, if the mitochondrial disease is nuclear-coded, the disease can be inherited as an autosomal dominant, autosomal recessive or X-linked trait.
The first symptoms usually show up in childhood or adolescence. In acquired mitochondriopathies, it is assumed that the cell organelles lose their function due to environmental influences. What environmental influences these are, however, has not yet been clarified. Often there are also mixed forms. This means that there is a hereditary predisposition, but this is only activated by environmental influences.
The main task of the mitochondria is to generate energy through the burning of fatty acids, the breakdown of acetyl-CoA and through oxidative phosphorylation. Due to the mutations, disturbances occur during the citric acid cycle or during fatty acid oxidation. This means that less energy is available. Since the enzymes of the respiratory chain, which can be impaired in mitochondrial disease, occur in a tissue-specific manner, only one or two organs can be affected by the disease.
Symptoms, ailments & signs
Mitochondriopathy can affect more than fifty enzymes within the mitochondria. As each of these enzymes has different tasks, the symptoms are correspondingly diverse. However, there are typical symptom constellations.
In chronic progressive external ophthalmic oplegia (CPEO), there are eye movement disorders. The eyelids droop (ptosis). This form of mitochondrial disease does not begin until the age of 20 to 40 years. If there is also paralysis of the external eye muscles and polyneuropathies or growth disorders, this is probably due to ophthalmoplegia plus (CPEOplus).
This form often flows into the Kearns-Sayre syndrome (KSS). In addition to the symptoms of CPEO, heart muscle diseases or changes in the retina also occur here. The disease of the heart muscle is characterized by conduction disorders. Another form of mitochondrial disease is myoclonus epilepsy with ragged red fibers (MERRF). Myoclonic epilepsy develops with progressive dementia and muscle weakness. The disease usually begins between the ages of 5 and 15.
Patients with MELAS syndrome are often short and suffer from migraines and / or diabetes mellitus. The onset of the disease is also between 5 and 15 years. The name MELAS syndrome indicates the typical clinical symptoms: mitochondrial encephalomyopathy, lactic acidosis and stroke-like episodes. Leber optic atrophy (LHON) is damage to the optic nerve with changes in the retina.
Here there is a painless loss of vision from the age of 20. Leigh syndrome manifests itself in the second or first year of life. The affected children are mentally retarded and suffer from muscle weakness. In addition, there is damage to the brainstem, which manifests itself in swallowing disorders or eye movement disorders.
Diagnosis & course of disease
The laboratory findings provide information about mitochondrial disease. Lactic acidosis becomes visible here. It is a lactic acid overload caused by the disruption in the citric acid cycle. As part of metabolic diagnostics, the organic acids in the urine and the amino acids in the blood serum are also determined. If the suspicion of mitochondrial disease is confirmed, a muscle sample can be taken by means of a muscle biopsy. The diagnosis can be confirmed here by the detection of so-called ragged red fibers. Evidence is provided by the Gömöri trichrome staining.
Complications
With mitochondrial disease, those affected usually suffer from various ailments. In most cases, the disease causes the affected person's eyelids to sag heavily, and thus to reduced aesthetics. This can have a negative effect on self-esteem and also lead to inferiority complexes. As a rule, the quality of life is significantly reduced by the mitochondrial disease.
It is also not uncommon for growth disorders and paralysis of the eye muscles to occur. Diseases of the heart muscle also occur, which in the worst case can be fatal. Those affected appear tired and exhausted and often suffer from migraines. Likewise, the risk of a stroke increases enormously, so that the life expectancy of the patient is also significantly reduced by mitochondrial disease.
This leads to muscle weakness and thus also to a reduced resilience. It is not uncommon for swallowing difficulties to lead to difficulties in taking food and fluids. A causal treatment of mitochondrial disease is not possible. Those affected are therefore dependent on a special diet and must avoid fear-inducing activities. There are various restrictions in everyday life.
When should you go to the doctor?
Irregular eye movements are a sign of an existing disorder. If the symptoms persist over a long period of time or if they increase in intensity, a doctor must be consulted. Since the disease begins at the age of 20, the symptoms that occur are alarming, especially in young adults. If there are visual changes in the shape of the eyes, there is cause for concern. If you have drooping eyelids or if you have problems with your eyesight, you will need a doctor. If the person concerned suffers from paralysis of the eye muscles, a doctor should be consulted. Growth disturbances and irregularities in the heart rhythm are further indications of the organism of a health impairment.
If the person concerned has the feeling that the heart is not working enough or if there is difficulty in breathing, a doctor's visit is advisable. General muscle weakness, poor performance and memory problems should be clarified by a doctor. Difficulty swallowing, short stature or an existing diabetes disease should be discussed with a doctor. If the person concerned perceives other irregularities, a check-up is recommended to check the general state of health intensively. Decreased vision from young adulthood onwards can be due to damage to the retina caused by mitochondrial disease. Sufferers are therefore strongly advised to consult a doctor in addition to an optician.
Therapy & Treatment
Mitochondrial diseases are usually hereditary, so that no causal therapy is possible. The production of energy is severely limited in mitochondrial disease. Therefore, those affected should consume as much energy as possible in the form of fats and glucose. A sufficient supply of minerals and water should also be ensured. Any physical condition that results in increased energy consumption should be avoided as far as possible. This includes sports, for example.
However, increases in temperature also go hand in hand with increased energy requirements. Fever should therefore always be reduced in patients with mitochondrial disease. Seizures also consume a lot of energy. Consistent therapy is required here. However, drugs that inhibit the respiratory chain must not be used. The respiratory chain is already impaired in mitochondrial disease and cannot tolerate any further restrictions. A very strong lactic acid overload can also be treated with buffer substances. Vitamins and cofactors can be used as a support.
Outlook & forecast
So far, patients with mitochondrial disease cannot be cured. A prognosis for those affected depends primarily on how early the first of the typical symptoms appear, how quickly the disease progresses, and how severe the seizures are. However, life expectancy and quality of life can easily be improved with an adapted therapy.
Whether a therapy helps and which treatment is indicated for mitochondrial disease is very different for each patient and also requires constant care by specialists who specialize in this disease. The symptoms of the disease usually show up in adolescence or early adulthood. Nevertheless, infants can also be affected by the disease. The earlier those affected fall ill, the faster the disease usually progresses.
In addition, the symptoms are often more severe in this case than in patients who become ill much later. In these cases, the disease usually progresses more slowly and with significantly milder symptoms. However, very severe and rapid courses are also possible in younger adults. Therapy options have increased significantly in recent years. Through newly researched methods in which the genetic material is analyzed, it is to be expected in the coming years that many of the mitochondrial diseases can be treated better.
prevention
In a large number of cases, mitochondrial disease is hereditary. Therefore, there is no effective prevention. However, some of the mitochondrial diseases are also favored by environmental influences. Since it has not yet been conclusively clarified which environmental influences can have a negative impact, there are currently no prevention proposals here either.
Aftercare
Treatment of mitochondrial disease must be continued permanently. Follow-up care focuses on providing the patient with the necessary therapeutic support. In addition, the intake of medication must be regularly checked and adjusted. Patients must consult the doctor at regular intervals.
The current state of health is discussed in conversation with the doctor. Any complaints should be clarified and alleviated by adjusting the therapy. Aftercare also includes constant diet adjustments. Since metabolic fluctuations occur in mitochondrial disease, different values such as pulse and blood pressure have to be measured again and again.
In addition, treatment with supplements must be monitored. The responsible nutritionist checks the effectiveness of the prescribed vitamins and adjusts the dose if necessary. Which measures are useful and necessary as part of the follow-up care depends on the respective symptoms. Basically, neuromuscular symptoms need to be monitored in order to detect complications at an early stage.
Further follow-up steps depend on the usually very variable course of the disease. Mitochondrial disease progresses rapidly, which is why most patients require medical attention several times a month. In severe cases, ongoing therapy is necessary.
You can do that yourself
Mitochondrial disease cannot be treated causally. Symptomatic therapy can, however, be supported by a number of strategies and measures.
If a fever occurs, appropriate measures must be taken to lower the body temperature. Classic methods such as cooling pads or yoghurt wraps have proven effective. A short walk in the fresh air can also help, provided the outside temperature is not too low. A doctor should definitely be consulted in the event of seizures. At the same time, first aid measures must be taken to alleviate the risk of injury from falls on the one hand and the cramps themselves on the other. If possible, the person affected should lie on their back and soothe the cramping part of the body with gentle massages. If the cramp occurs in several limbs, heat treatments can help. The symptoms usually subside after a few minutes if the affected muscles are consistently calmed and relaxed.
A good alternative from the household is St. John's wort oil. The herbal remedy mainly helps with mild cramps in the muscles and contributes to relaxation overall. Vitamins and minerals provide support. If symptoms persist longer than usual or if unusual symptoms occur, a doctor should be consulted.



.jpg)

















.jpg)



