Werlhof's disease, also as Werlhof disease and Immune thrombocytopenia known to be an autoimmune disease. It is characterized by the formation of antibodies against the body's own blood platelets (thrombocytes) in those affected. The disease requires extensive medical treatment and therapy.
What is Werlhof's disease?

© brgfx - stock.adobe.com
The general practitioner Paul Gottlieb Werlhof (1699-1767) first described Morbus maculosus haemorrhagicus as a disease of the blood in 1735. It was not until 1883 that it was diagnosed that the signs of the disease were generated by a decrease in blood platelets.
Werlhof's disease, the Werlhof disease, bears the name of its discoverer Paul Gottlieb Werlhof like so many others. A characteristic of the disease is that the body mistakenly attacks its own platelets, which leads to their rapid breakdown. This is why bleeding will occur if left untreated.
causes
Werlhof's disease belongs to the group of autoimmune diseases: The immune system forms antibodies against the body's own blood platelets, the thrombocytes. They are components of the white and red blood cells and play an important role in blood clotting because the disc-shaped platelets can close wounds through cross-linking.
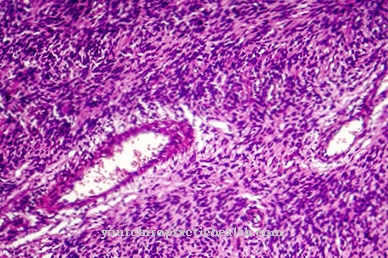
In Werlhof's disease, the number of platelets decreases significantly because the blood platelets that are overloaded with antibodies are broken down too quickly in the spleen. While the platelet count in the laboratory is an average of 140 to 360 thousand / μl, the tendency to bleeding increases as the platelet concentration in the blood decreases. Petechiae are the typical appearance.
Petechiae are punctiform hemorrhages the size of a pinhead from the capillaries of the mucous membranes or the skin. Initially, the petechiae are usually noticeable on the lower leg or on the ankles. If the cause of the bleeding is the lack of platelets, it is called thrombocytopenic purpura.
If the proportion of platelets decreases dramatically, one speaks of primary immune thrombocythemia. This deficiency can reach life-threatening proportions. In addition, the trigger of the primary immune thrombocythemia is not known according to current knowledge. Studies have shown that Werlhof's disease often has to be diagnosed after infections and / or pregnancy.
In children, the disease occasionally occurs spontaneously, only to heal spontaneously after a while. This positive course can also be observed in adulthood, but only in the first year of illness. After a year, Werlhof's disease becomes chronic.
Symptoms, ailments & signs
In Werlhof's disease, there is a sharp decrease in blood platelets (thrombocytes). As a result, the smallest injuries in the blood vessels can no longer be closed, so that blood leaks out of the arteries and veins. The clinical picture of Werlhof's disease is correspondingly diverse.
In the initial phase, small punctiform bleeding, so-called petechiae, is one of the characteristic symptoms. These can appear on the skin as well as on the mucous membranes. The resulting skin or mucous membrane hemorrhages are roughly the size of a pin and are often mistaken for flea bites.
If the number of blood platelets continues to decrease, the bleeding can expand and the individual petechiae flow together to form flat skin manifestations. Large bruises (hematomas) occur even with minor injuries. Heavy nosebleeds and bleeding that can hardly be stopped from minor cuts or abrasions also indicate a reduced number of platelets in the blood.
Women may also have vaginal bleeding. Blood can also appear in the stool in both men and women. Pronounced Werlhof's disease with bleeding in internal organs such as the spleen, liver, lungs or kidneys can also result in life-threatening shock.
Diagnosis & course
A steadily and sharply decreasing number of blood platelets means that injuries to the blood vessels cannot be closed again. This leakage of blood generates several symptoms:
In the beginning there are the pinhead-sized petechiae. When they flow together, extensive bleeding occurs. Bruising, heavy nosebleeds, blood in the urine and stool, vaginal bleeding, and vomiting blood are typical symptoms. If the bleeding occurs heavily, acute shock symptoms can occur.
If the organism is supplied with too little oxygen, whereby blood loss can be a significant cause in Werlhof's disease, the body begins to exclude organs from the oxygen supply that are unnecessarily unimportant. This condition can become life-threatening if left untreated. If the brain, lungs, liver, spleen or other internal organs are affected, massive damage and functional disorders can also occur.
Werlhof's disease can be identified on the basis of the blood count, because the number of platelets is significantly reduced. After examining the bone marrow, however, the doctor will diagnose a significant excess of hematopoietic megakaryocytes. Other platelet diseases must therefore be excluded in the course of the diagnosis.
Complications
With Werlhof's disease, patients experience significant restrictions and complaints in everyday life. In most cases, there is increased bleeding, which can also occur internally. Without treatment, life expectancy is significantly reduced because the organs can be damaged, which is irreversible.
Nosebleeds and a reduced resilience of the person affected are also not uncommon. The blood is also found in stool or urine and can lead to panic attacks or sweats in many people. In addition, it is not uncommon for those affected to vomit blood. The body is also insufficiently supplied with oxygen, and the internal organs can also be irreversibly damaged.
The liver and spleen in particular can lead to a life-threatening condition for the patient. The damage to the organs leads to further complaints and complications. Treatment of this disease takes place acutely with the help of drugs. There are usually no complications.
In severe cases, surgery or an organ transplant may be necessary to keep the person alive. This may also reduce the patient's life expectancy.
When should you go to the doctor?
If the person concerned suddenly suffers from rapid bruising or discoloration of the skin, there is cause for concern. A doctor is required in the event of dizziness, increased blood loss, disorders of the blood circulation or a decrease in exercise capacity. If you have difficulty concentrating, heavy bleeding in the case of minor injuries, a repeated taste of blood in your mouth or blood in the excretions, you need to see a doctor.
An internal weakness, general malaise or feeling of illness should be examined and treated. Bruising, abnormalities in the female cycle or uncontrolled bleeding from the vagina are warning signals of the organism. There is a medical condition that needs to be diagnosed and treated as soon as possible. Consultation with a doctor should be sought in the event of changes in the mucous membranes, pale skin or increased sensitivity to cold stimuli.
Since the disease can lead to bleeding of the organs and thus to a life-threatening condition, a visit to the doctor is recommended as soon as the first abnormalities appear. If there is an acute health-threatening condition, an ambulance service is required. An emergency doctor must be called and, at the same time, first aid measures must be initiated by those present to ensure the survival of the person concerned.
Treatment & Therapy
Does the doctor have the Werlhof disease established, use different methods of treatment. The immediate focus is primarily on stopping acute bleeding. For this purpose, high-dose corticosteroids are used as part of “first-line therapy”. This shock therapy, which has side effects, ends after a relatively short time and can result in a thorough regression of the disease symptoms after just a few weeks.
Children with mild disease do not have to undergo this therapy. Werlhof's disease usually occurs here as a result of viral infections or occasionally after mumps, measles or rubella vaccinations for a short time, in order to then heal independently. Chronic courses in adults are treated with antibodies, so-called immunoglobulins, for example biological rituximab or other immunosuppressants. This is how the autoimmune disease is to be combated.
Manifest clinical pictures are met with the surgical removal of the spleen. The advantages of a healing of the Werlhof disease must be weighed against the possible complications during the operation. Despite the removal of the spleen, relapses occur and the risk of dying is around one percent.
You can find your medication here
➔ Drugs for wound treatment and injuriesOutlook & forecast
In general, the prognosis for Werlhof's disease in adults is favorable and the overall cure rate is between 70 and 80 percent. For an exact prognosis, however, a distinction must be made between acute and chronic forms.
In the case of acute Werlhof's disease, in most cases a complete remission (= relief of symptoms) occurs within one month. This is especially true for affected children. In the case of chronic courses, on the other hand, spontaneous remission only occurs in rare cases (less than 5 percent). This value improves considerably with steroid therapy and increases to 25 percent, with the addition of further therapeutic measures even to two thirds. Around 0.4 percent of adults with severe chronic Werlhof's disease before the age of 40 die of intracerebral bleeding (bleeding in the brain tissue). This probability increases with age and is 1.2 percent for 40 to 60 year olds and 13 percent for those over 60.
In addition, recurrences (recurrence of the symptoms) often occur in Werlhof's disease. In these cases, the specialists often consider surgical removal of the spleen (splenectomy). However, even removing the spleen does not completely neutralize the risk of recurrence.
prevention
Since the exact cause of Werlhof's disease is currently still being researched and the disease is also an autoimmune disease, preventive measures are not yet known.
Aftercare
In most cases, those affected by Werlhof's disease do not have any special or direct follow-up measures available, so that those affected with this disease should ideally consult a doctor very early to prevent other complications and complaints from occurring. Since this is a genetic disease, it usually cannot be completely cured.
Therefore, those affected should seek advice, especially if they want to have children, so that the disease does not recur in their descendants. As a rule, those affected by Werlhof's disease are dependent on the intake of various drugs. The correct dosage and regular intake should always be observed, whereby a doctor should be consulted if there are any questions or if anything is unclear.
Many of those affected are also dependent on regular controls and examinations of their internal organs. In this way, other damage can be identified and treated early on. It is not uncommon for people to be in contact with other people affected by the disease, as this can lead to an exchange of information. This information can make the patient's everyday life easier.
You can do that yourself
The sick person cannot treat Werlhof's disease themselves. However, the symptoms and complaints of the autoimmune disease can be alleviated through targeted measures and a change in lifestyle. The typical skin changes can be covered with make-up or covered with the right clothing. This is especially necessary in the later stages of the disease, when the bleeding and scarring have already spread to the entire arms and neck. If severe bruises suddenly appear, these can be cooled with the help of wraps or cold packs.
In the long term, the sick have to change their diet. This makes the immune system more resistant to infection. In addition to medication prescribed by a doctor, natural remedies such as aloe vera, sage, devil's claw or ginseng can help with reddened eyes, bleeding gums and vomiting blood.
If the measures mentioned do not alleviate the symptoms and complaints of Werlhof's disease, the doctor must be consulted again. The medication may need to be adjusted or there is another condition that needs to be diagnosed. Attending a self-help group makes it easier to deal with the disease and can thus contribute to a higher quality of life.




















.jpg)



