The Myositis or Inflammation of the muscles can be hereditary or caused by various pathogens. Infections, immune disorders, parasites, viruses, bacteria or toxins can trigger such muscle inflammation. This complicates both the diagnosis and the therapy of myositis.
What is Muscle Inflammation?
.jpg)
© Dmitry_Tkachev - stock.adobe.com
As Muscle inflammation or myositis is the name given to all inflammatory diseases of the muscles of the human skeleton. A distinction is made between different forms of myositis. The main ones are known as polymyositis, inclusion body myositis, or dermatomyositis.
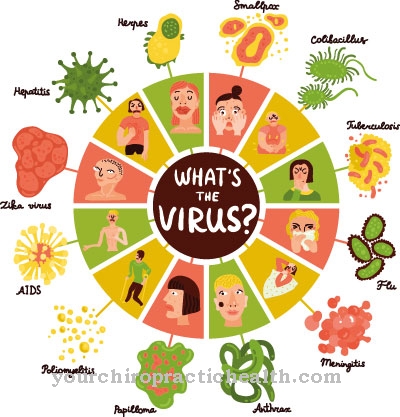
Myositis can also be triggered by various bacterial or viral pathogens or infections as well as by injuries to muscles. Myositis also sometimes occurs for hereditary reasons, such as Münchmeyer syndrome. It can also arise as a result of exposure to poison. Myositis is a relatively rare disease in our part of the world.
Inclusion body myositis is most common in adults over the age of 50. However, dermatomyositis is more common in the general population. Interestingly, both forms of myositis occur preferentially in children and adolescents and then again after mid-life.
Such muscle inflammation can be accompanied by weak muscles in certain areas of the body, skin symptoms or swallowing disorders. The course of myositis can be easily treated. However, the myositis can also progress and require permanent hospital treatment.
causes
A Myositiscaused by certain parasites as well as bacterial or viral pathogens is rarely found in our latitudes. Muscle inflammation is much more common when there is an inflammatory system disease.
Inflammatory rheumatic diseases or connective tissue diseases can also lead to muscle inflammation. In polymyositis and also in dermatomyositis, an auto-immune disease is assumed to be the cause of the muscle inflammation. Inclusion body myositis, on the other hand, is attributed to degenerative and inflammatory processes.
Typically, elevated levels of certain inflammatory parameters and enzymes are often found in patients with myositis. However, these enzymes are not the cause of myositis. They arise in the muscle fibers and are increasingly released by the muscle inflammation. Therefore, these enzymes can be used as diagnostic tools for determining myositis.
Symptoms, ailments & signs
The clinical spectrum of myositis is quite extensive and, depending on the form and severity, ranges from mild joint pain to neurological symptoms. In the early stages of the disease, patients with polymyositis mainly complain of unspecific complaints such as tiredness and fatigue.
A fever can also occur. A characteristic symptom of polymyositis is a sore muscles-like feeling in the muscles of the arms and legs. This pain occurs regardless of whether the patient has moved a lot or little. Many patients also complain of pronounced muscle weakness. This always occurs progressively and symmetrically, i.e. on both sides of the body.
People with myositis find it difficult to raise their arms or have restricted movement of the legs and head. In both poly- and dermatomyositis, not only the muscles but also internal organs can be impaired in their function. If the striated muscles of the larynx and / or the lungs are affected by the disease, swallowing difficulties and shortness of breath occur.
In dermatomyositis, in addition to the muscular impairments, various skin symptoms appear. These can vary in intensity and in individual cases even be completely absent.
Course of disease
Before treating the Myositis diagnostics must be in place. With an electrical voltage measurement, a muscle biopsy or electroneurography, one can track down myositis as well as with the measurement of the enzyme values in the muscle fibers.
What makes the diagnosis of myositis more difficult is the fact that muscle inflammation - depending on the form - can develop over months or years. It is now known that patients with dermatomyositis are more likely to develop malignant or malignant tumors. Necrosis or immigrated inflammatory cells can provide important information about the course of the disease.
Each form of myositis has its own diagnostic criteria. Still it is difficult to determine. The disease progresses slowly and is often only noticed at an advanced stage. In addition, diseases such as muscular dystrophy can make diagnosis difficult.
Complications
Muscle inflammation can cause a variety of complications. First of all, the myositis leads to symptoms such as aching limbs, fatigue, fever and loss of appetite, which worsen general well-being and can result in dehydration or nutritional deficiencies. Prolonged illness is often associated with being bedridden. The resulting immobility can trigger depressive moods and cause eczema and inflammation in older patients.
Sometimes the muscle inflammation can spread to surrounding areas of the body and cause serious complications. For example, if it spreads to the ankle, it can encapsulate and eventually stiffen. If left untreated, muscle inflammation will get progressively worse. This can lead to muscle damage and, as a result, even symptoms of paralysis.
If the affected muscle can no longer be moved as before, this can lead to psychological complaints. Treating muscle inflammation also carries risks. The prescribed antibiotics and cortisone preparations can cause side effects such as diarrhea and skin irritation. An intolerance can lead to joint pain, serious intestinal diseases and depression. Paralysis and muscle injuries can cause hardening, which, if not handled properly, can lead to tissue damage.
When should you go to the doctor?
Intensive sport or other physical activity can lead to pain or a decrease in normal performance. A doctor's visit is normally not necessary. If the symptoms reduce within a few hours or after a good night's sleep, no doctor is required. With sufficient rest and protection, the organism uses the time it needs to regenerate. After a short time you are expected to be free of symptoms.
Consult a doctor if you experience pain or other discomfort with normal, everyday movements. If the symptoms persist for several days and weeks or if they become more intense, a doctor's visit is advisable. A doctor should be consulted if there are signs such as restricted mobility, tiredness, increased body temperature or decreased physical exertion. If there is an inner irritation, a relieving posture of the body or a crooked posture, a visit to the doctor is recommended. Changes in the appearance of the skin, sensitivity to pressure or increased sensitivity to temperature influences must be examined and treated.
Impairments to breathing are of particular concern. If symptoms occur during the natural act of swallowing or if breathing is difficult, a doctor should immediately clarify the symptoms. In these cases, the muscle problems lead to an impairment of the organ activity of the lungs and must be treated medically.
Treatment & Therapy
Depending on the shape and severity of the Muscle inflammation you have to treat differently. The administration of high-dose cortisone preparations has proven to be the standard treatment for muscle inflammation of the dermatomyositis or polymyositis type.
Depending on the type of myositis, the symptoms improve and the cortisone can be reduced after a few weeks. Sometimes the course of myositis cannot be positively influenced even with cortisone. So-called immunosuppressants or immunoglobulins are then used. They suppress the immune system in its overreactions.
Patients with inclusion body myositis are treated with physical therapy or occupational therapy. The course of this myositis often requires treatment in a clinic that specializes in neuromuscular diseases. In the case of paralysis or muscle injuries, hardening can develop, which necessitates more specific treatment of the myositis.
You can find your medication here
➔ Medicines for muscle painOutlook & forecast
The prognosis for a muscle inflammation depends on the cause, the type of treatment and the duration of the inflammation. No uniform statements can be made on this.
If, for example, autoimmune diseases are responsible for the muscle inflammation, weeks of therapy are usually necessary in order to produce an improvement. In addition, such causal diseases are always chronic, which is why lifelong therapy is necessary on the one hand and myositis can recur on the other. In such cases, the prognosis is all the better if those affected can keep their muscles healthy for a long time thanks to good exercise and well-controlled medication.
If local infections or other inflammations are the trigger, the success of the therapy determines the prognosis. So it can sometimes take several weeks before there is any improvement. The problem with muscle inflammation, however, is not the pain, but the failure symptoms that occur later. The muscles can become undersupplied or atrophy as a result of inflammation. Avoiding exercise because of pain also leads to muscle wasting.
It is believed that those affected are often weakened after surviving myositis and need exercise therapy to rebuild the muscles. Muscle damage as a result of acute myositis is considered to be easily reversible.
prevention
A prevention against the development of a Myositis is practically impossible. You can protect yourself against viral, bacterial or parasitic pathogens to a certain extent, but you could still get myositis through other circumstances. Nothing can be done preventively against an autoimmune disease or toxic myositis.
Aftercare
The disease myositis requires lifelong treatment, as it is not curable according to current scientific standards. As part of the aftercare, the aim is to inhibit the inflammation and to minimize the weakening of the muscles and to maintain the mobility of the skeletal muscles concerned.
This requires a follow-up, the extent of which depends on the extent of the complaints. Doctor and patient make regular appointments. The prescriptions required for drugs such as cortisone and immunosuppressants as well as for physiotherapy and occupational therapy are issued in these. Rehabilitation is often ordered immediately after the diagnosis.
Under professional guidance, the patient learns what consequences myositis has for his life and how he can counter them. However, for the measures to be successful, the inflammation must have largely healed. A follow-up examination always includes a discussion about the complaint situation. Everyday professional and private life can be particularly difficult.
Possible offers of help will be discussed if necessary. In addition, a blood test is carried out to determine inflammation parameters. This enables the doctor to document the progress of the disease and adjust the therapy if necessary. The success of the treatment depends crucially on the willingness of the patient to cooperate. Long periods of rest not infrequently lead to the loss of muscle functions.
You can do that yourself
Muscle inflammation usually requires extensive medical treatment. In addition, the patient can take some measures to alleviate the symptoms.
First of all, the affected muscle should be spared. For severe pain, warm pads and accompanying measures such as soothing teas or gentle massages are recommended. A bandage can also contribute to a speedy recovery. Physiotherapy and occupational therapy are important components of therapy. The patient can support these measures at home with moderate exercise and individual exercises. The type of workout is best determined in collaboration with a sports doctor. If the muscle inflammation is accompanied by paralysis, muscle injuries or hardening, further measures must be initiated. Drug therapy is usually started, supported by massages and alternative methods from Chinese medicine. In consultation with the doctor, acupuncture can also be used.
Muscle inflammation usually heals within a few days to weeks. If the symptoms persist over a longer period of time, treatment in a clinic may be necessary. Those affected should inform the doctor of any complaints and suggest that they change the drug administration in the event of side effects or interactions with the prescribed medication.





















.jpg)



