All processes of the formation of new blood vessels that take place in the organism of an adult person are summarized as vascularization, especially angiogenesis. The Neovascularization In contrast, it is more known as a pathological and thus pathologically excessive formation of new vessels. This new formation takes place, for example, in the context of cancer and is used to supply tumors with nutrients and oxygen.
What is Neovascularization?

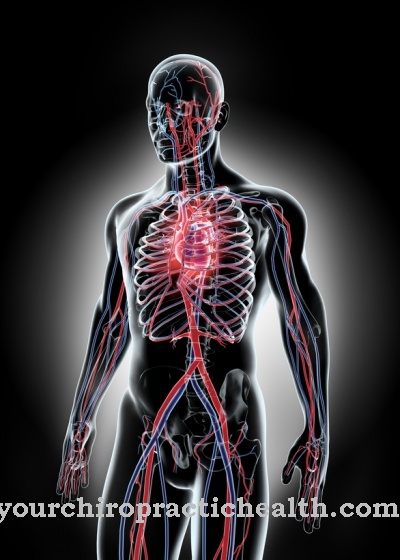
As part of the so-called vascularization, smaller blood vessels form. Vascularized tissues therefore carry a particularly large number of blood vessels and bleed much more heavily after injuries, which benefits wound healing.
Physiological processes of the formation of new vessels are summarized under the technical term of angiogenesis. In angiogenesis, new blood vessels grow in processes of splitting and sprouting from existing blood vessels, for example to bypass constrictions. In addition to the shear forces in the vessels, these processes depend primarily on the blood concentration of immunological monocytes. Vascularization can be used synonymously with angiogenesis or denotes the whole blood supply to a tissue or organ.
Neovascularization is used as a generic term for all new vessel formations in an adult organism. Since in the adult organism, apart from wound healing, the formation of new vessels is usually associated with pathological phenomena, the term neovascularization is usually also used to describe a disease.
In this context, neovascularization always occurs when an angiogenic process is not a physiological but a pathological process. Accordingly, excessive neovascularization in the context of tumor diseases or macular degeneration is referred to as neovascularization. Physiological neovascularization in the adult organism is referred to as vascularization rather than neovascularization, although in fact it is newly formed.
Function & task
During angiogenesis, new vascular structures with endothelial cell lining and smooth muscle cells and pericytes are formed. Angiogenesis is a wound healing process that should not be underestimated. The blood supplies all body tissues and organs with nutrients and oxygen. In addition, messenger substances reach the individual tissues via the blood. The cells of the immune system are also transported via the blood. The blood connection of a tissue is therefore vital.
In this context, angiogenesis ensures the survival of tissues whose blood connection has been disrupted due to injuries. Together with the term vascularization, the term angiogenesis has meanwhile established itself as an umbrella term for all forms of new vessel formation in the adult organism. In addition to the wound healing process described, there is, for example, vasculogenesis, in which vascular structures are newly formed based on circulating stem cells or angioblasts, which become endothelial cells.
During arteriogenesis, arteries and smaller arterioles are formed and, through the recruitment of smooth muscle cells, they obtain full-fledged vascular walls. Essentially the same process occurs in the formation of new veins.
All of the above-mentioned new blood vessels are vascularizations and are sometimes based on the release of the growth factor VEGF. During neovascularization, there is a locally limited overproduction of VEGF. This overproduction can be attributed to the release by tumor cells, for example. When the tumor disease progresses, the tumor cells initiate neovascularization so that the growing, progressively spreading tumor is adequately supplied with blood and thus receives enough oxygen and nutrients to grow.
In this context, the blockade of the neovascularization can stop the growth of the tumor. This principle is used in anti-angiogenic tumor therapy to treat patients with cancer.
Illnesses & ailments
Neovascularizations occur in the context of numerous tumor diseases. Excessive neovascularization does not always have to be associated with excessive VEGF production, but with a tumor. Many other pathological processes can be to blame for excessive vascularization, especially when there are new blood vessels in the eye. For example, exudative “wet” macular degeneration or diabetic retinopathy, which is also known as proliferative retinopathy.
In addition, neovascularization takes place in the context of neovascularization glaucoma and also occurs accompanying retinopathia prematurorum. Corneal neovascularization is also frequently observed in patients with contact lenses.
Depending on the cause, abnormally excessive vascularization processes are treated differently. To weaken angiogenesis, anti-angiogenetic therapy is usually carried out, in which the patient receives, for example, VEGF-neutralizing monoclonal antibodies. Treatment with bevacizumab or rhuMAb-VEGF, for example, has been approved for patients with metastatic colon cancer and is intended to block the formation of new blood vessels, which ultimately also blocks the growth of the tumor.
The active ingredient bevacizumab is now also used for breast cancer, kidney cancer and lung cancer. In addition, there are now anti-angiogenic therapies with the antibody ramucirumab, which binds to the VEGF R2 receptor and in this way blocks the receptor for the angiogenic growth factor VEGF R2. The blockage prevents the formation of blood vessels, as the formation is only stimulated by the receptor-growth factor complex, which now no longer takes place. So far, ramucirumab has mainly been used in the treatment of gastric cancer.
The situation is different with the therapy of excessive neovascularization that is not associated with tumor diseases. In the case of neovascularization in the context of contact lens use, the focus of therapy is the suspension of contact lens use. In addition, topical drugs are used to regulate angiogenesis. These drugs are usually eye drops. The main active ingredients used are steroids and GS-101. The latter substance is an antisense oligonucleotide.