To understand what a nosocomial infection means, the layman must first visualize the meaning of the word from ancient Greek. "Nosos" means "illness" and "komein" means "care" and the word "nosokomeion" stands for the ancient Greek premises of health resorts. A nosocomial infection means nothing else than one Hospital infection.
What is nosocomial infection?

© auremar - stock.adobe.com
Nosocomial infections are an increasing problem in hospitals and care facilities and constitute a large part of all serious complications there.
The quality of nursing and medical care for the patient suffers greatly from the increase in nosocomial infections and the patient's stay is extended by up to four days on average, which leads to major financial losses in the clinics, which have to settle according to "case-by-case flat rates" .
In Germany, an estimated 20,000 people die every year from nosocomial infections and a further 500,000 people become infected with pathogens, most of which are already resistant to many common antibiotics. These include multi-resistant Staphylococcus aureus or particularly difficult to treat E.coli and Klebsiella strains.
causes
Although the Infection Protection Act in Germany stipulates that hospitals, dialysis facilities, medical practices and day clinics must use the latest medical and scientific knowledge nosocomial infection have to prevent, this is not necessarily checked.
For this purpose there are guidelines from the Commission for Hospital Hygiene and Infection Prevention from the Robert Koch Institute, as well as recommendations for resistances and therapies that hospitals must observe in order to prevent the distribution of resistant pathogens through nosocomial infection.
In many cases, hospital germs are spread through human contact, which is why hand disinfection is mandatory when entering and leaving the room. Qualified cleaning and disinfection of all rooms is also essential, especially in the operating theater, in order to avoid nosocomial infection.
Symptoms, ailments & signs
Nosocomial infections can cause different symptoms depending on the area of the body affected. The most common general symptoms include fever, cough, headache and aching limbs, as well as pain and pus formation on joints or surgical wounds.
Infections with multi-resistant germs (MRSA) in particular do not respond to conventional antibiotics and therefore cause fever and a general feeling of illness. In the worst case, these pathogens can get into the bloodstream and cause life-threatening sepsis (blood poisoning).
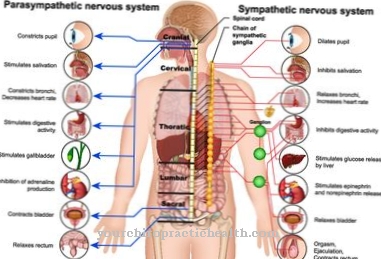
Patients who are supplied with a urinary catheter often suffer from a bladder infection, since infectious agents can rise into the bladder via the catheter tube. The infection can manifest itself as a fever or pain in the back. One of the most common complications during a hospital stay is catheter-associated infection.
Bacteria or fungi migrate from the skin along a vascular catheter into the vessel and cause inflammation there. Nosocomial infections are also manifested by cough, fever, chest pain and shortness of breath. These are almost always signs of pneumonia. Pain, swelling, redness, warmth and above all pus formation indicate a wound infection after an operation.
Diagnosis & course
A nosocomial infection triggers a wide variety of clinical pictures. In intensive care units, the so-called "ventilation-associated pneumonia" is particularly noticeable, from which 30,000 people in intensive care units in Germany fall ill every year.
Another nosocomial infection is "catheter-associated urinary tract infection". Statistically, this is probably the most common nosocomial infection. A dreaded complication of such urinary tract infections is a generalization of germs from the urinary tract into the whole body, which can lead to sepsis or septic shock.
Venous catheters are another possibility of contracting a nosocomial infection, but these are indispensable for many patients - be it for parenteral nutrient supply or the administration of medication. Wound infections that occur after operations because germs penetrate the unprotected area are also very common.
Complications
The complications and the further course of this disease usually depend very much on the exact infection. For this reason, no general forecast can be made about the course. However, severe infection or blood poisoning can result in death if the infection is not treated. However, the infections can be avoided relatively easily with hygiene measures, so that the patient rarely dies.
In many cases, those affected also suffer from urinary tract infections, so that it comes to burning pain when urinating. Infections and inflammations on wounds are also common and can delay wound healing. However, early diagnosis and treatment can limit and treat all of these symptoms so that there are no further complications.
The patient's life expectancy is also usually not reduced with the right treatment. The treatment itself is mostly done with the help of antibiotics and leads to success relatively quickly. However, the patient is still indicated for a longer stay in the hospital.
When should you go to the doctor?
Nosocomial infection is a dangerous infection because the patient's body is likely to be weakened by the existing illness that initially brought him to the hospital. Furthermore, depending on the pathogen, the immune system is on its own in the fight, since the pathogens can be immune to known active substances. Nevertheless, a nosocomial infection belongs in the hands of a doctor, which is usually given by the fact that symptoms of the infection show up while the patient is still in the hospital. This is the best possible case, because it allows the infection to be detected promptly and treatment can be initiated.In addition, the person concerned is under constant medical supervision and can therefore be quickly intervened if his condition worsens.
However, if signs of infection appear after discharge from the hospital, the patient should contact the doctor immediately. Especially if you have symptoms immediately after an operation, there is nothing to prevent you from going to the emergency room. Although it can be a nosocomial infection, it can also be an infection of the surgical wounds with a pathogen that has not developed immunity to common active ingredients. In any case, the doctor must clarify the cause and treat the infection quickly, since the patient's body is now very weak.
Treatment & Therapy
To a nosocomial infection To be able to treat effectively with the right antibiotics, microbiological examinations are essential. For this purpose, the appropriate samples are taken, applied to culture media and examined for sensitivity to antibiotics.
The nosocomial infection is treated according to the so-called "antibiogram", whereby in urgent cases antibiotic combinations are administered as a preventative measure. If pneumonia is suspected, the doctor flushes out the lungs with saline solution and sucks off the secretion obtained, thereby gaining the so-called "bronchial lavage", which in the positive case contains the bacteria that cause the disease.
In order to determine urinary tract infections, a urine sample is required, which is immediately applied to a nutrient medium and incubated. "Catheter-associated venous infections" can quickly lead to sepsis, which can be detected by means of a "blood culture".
A nosocomial infection with Candida species or Staphylococcus aureus, which results in high mortality, is particularly dangerous. The typical wound infection after operations can be detected with a smear from the affected area; Staphylococcus aureus and the multi-resistant representatives of this species are particularly common here.
Outlook & forecast
The prognosis of the hospital infection must be assessed according to the individual circumstances. The cause of the infection and the pathogens must be clarified in order to be able to assess the further course. In addition, the general state of health of the person affected must also be taken into account when making the overall prognosis.
Naturally, people are in a hospital, on nursing wards or under intensive medical care because they have already suffered an underlying disease and have a weakened immune system. This often complicates the treatment options and worsens the further course. In risk patients, therefore, mostly harmless germs can lead to serious health consequences. It is therefore possible that a nosocomial infection could develop into a life-threatening condition. The number of people who die from hospital infections each year is around 30,000. The organism is often so weakened that it can no longer adequately defend itself against infections of all kinds.
The prognosis is significantly improved if the person concerned has a fundamentally healthy and stable immune system and the underlying disease can be classified as not of much concern. With a healthy lifestyle, a balanced diet and sufficient rest, recovery can be achieved. It is also necessary to clarify the germ that has been obtained and to provide adequate drug therapy.
prevention
Since it's not the one nosocomial infection every disease is specially prevented. "Ventilation-associated pneumonia" requires strict hand hygiene before any activity on the ventilation system as well as a semi-upright lying position of the patient at a 30 ° angle.
Since with venous catheters an external colonization of the catheter tip often triggers the nosocomial infection, there are catheters that are impregnated with antibiotics. A nosocomial urinary tract infection sometimes does not even occur if disposable catheters are used instead of long-term urine drainage. The aim is to push back nosocomial infections like in the Netherlands as far as possible in Germany and to create a better understanding of hygiene among hospital staff.
Aftercare
Nosocomial infections are infections caused by so-called hospital germs. These pathogens are often multi-resistant to antibiotics. Acute therapy is difficult and, depending on the infection, long-term consequences for the patient cannot be ruled out. Follow-up care of the nosocomial infection is therefore difficult.
On the one hand, it must be clarified whether the acute illness could be cured and whether the pathogens have permanently disappeared from the patient's body with certain strong drugs. On the other hand, long-term effects on organs or metabolism must be taken into account. Long-term after-effects from the drugs used must also be treated and treated in the aftercare.
The attending specialist will ensure the blood parameters and vital functions as well as the organ function of the organ or organs affected by the infection at regular intervals. In the case of nosocomial infection, there can be long-term effects, such as impairment of the heart or lung function. These complications must be ruled out and require strict follow-up monitoring.
A certain recovery time after the acute treatment is also essential for the patient - the specialist should advise accordingly and take enough time for the patient and his questions.
You can do that yourself
Depending on the type and severity of the nosocomial infection, patients can do a few things themselves to alleviate the symptoms and discomfort. First of all, the body needs a lot of rest. Those affected should take a few days off and especially consume light foods during the illness.
General measures such as drinking a lot and avoiding alcohol and cigarettes help with recovery. In addition, other people should be avoided for a certain period of time in order to avoid infection. If you have a sore throat, lozenges or saline solutions for inhalation help. The natural remedy Echinacea strengthens the immune system and can be taken either as a tea or as a plant juice. In the case of a bacterial infection, strict personal hygiene also helps.
If the symptoms do not go away despite everything, the family doctor must be consulted. It is important to determine the causative pathogen, for example through research in the hospital in which the pathogen for the nosocomial infection was received. There may be a serious infection that needs to be treated with medication in addition to self-treatment. Patients should discuss with their family doctor which measures will best help against their individual complaints.