Opsonin is the umbrella term for various proteins. Opsonins occur, for example, as antibodies or complement factors and as such are involved in the body's immune response. Opsonins play a role in numerous diseases, including both autoinflammatory diseases and infections.
What is opsonin?
In biology, opsonins are various proteins that belong to the immune system. They include antibodies and complement factors, among others. Both are necessary for the defense against pathogens.
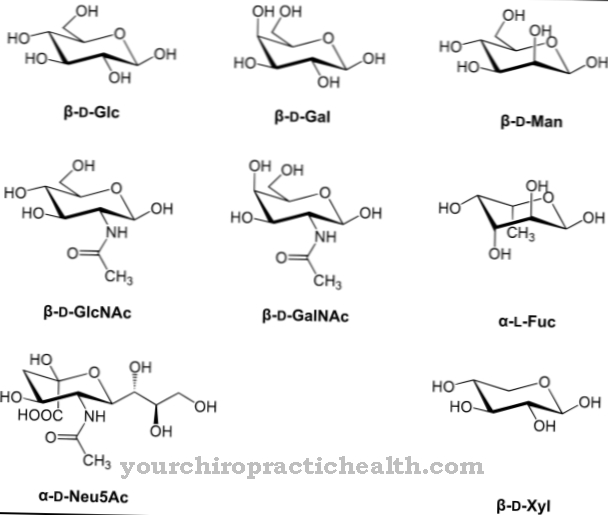
The name opsonin is derived from the Greek "opsôneîn", which means something like "prepare for food": Opsonins prepare microorganisms for the phagocytes. Phagocytes are scavenger cells that can eliminate tissue, bacteria, fungi, parasites or viruses. The opsonins function partly as markers (e.g. antibodies), partly they help the phagocytes to bind to the dangerous cells (e.g. fibronectin).
Opsonins can be divided into three groups: Antibodies attach to antigens and signal to the immune system that a potential pest is present. Complement factors in turn react to the antigens. The third group of opsonins circulates freely in the blood.
Function, effect & tasks
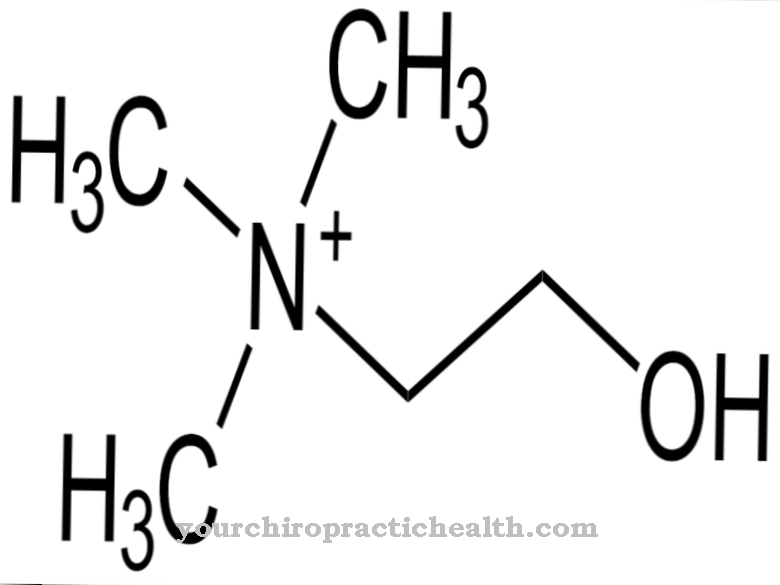
The antibodies of the immune system are a variant of the opsonins. Antibodies are soluble blood proteins that can bind to antigens. Antigens are structures on the surface of cells that provide information about the type of cell. The immune system uses the antigens to recognize foreign bodies and identify pathogens. Antibodies mark the suspicious objects and thus enable a defense reaction.
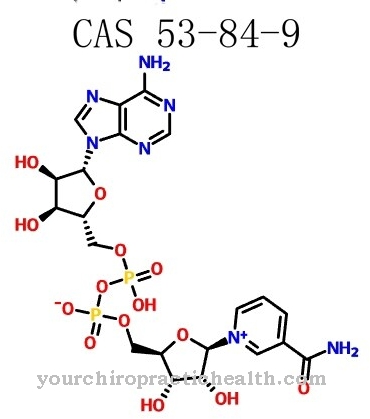
The complement factors of the immune system also belong to the opsonins. The complement system consists of plasma proteins that are either dissolved in the blood or bound to cells. They are primarily involved in the immune reaction to microorganisms such as fungi, bacteria or parasites. To do this, the complement factors attach themselves to the intruder and cover its surface. Biology calls this process opsonization. The opsonization signals the dangerousness of the opsonized object and stimulates the phagocytes to ingest and digest it.
Fibronectin is a non-specific opsonin. It occurs in the extracellular matrix and is involved, for example, in tissue repair, cell migration and adhesion, and hemostasis. Fibronectin has a mediating function in the immune reaction: it helps phagocytes to bind to antigens.
Another opsonin is the C-reactive protein (CRP), which is one of the acute phase proteins: the body produces it in larger quantities when there is an acute infection or inflammation. CRP activates the complement system. PTX3 also has a similar function - but the receptor not only reacts to various bacteria, fungi and viruses, but also to the body's own cells, which pose a threat.
Cells that are severely damaged or contain a virus initiate their own destruction as soon as they recognize the risk and cannot eliminate it in any other way. This cell suicide is also known as apoptosis. PTX3 also targets such cells, helping to clear them away from the phagocytes before damaging cells spread.
Education, occurrence, properties & optimal values
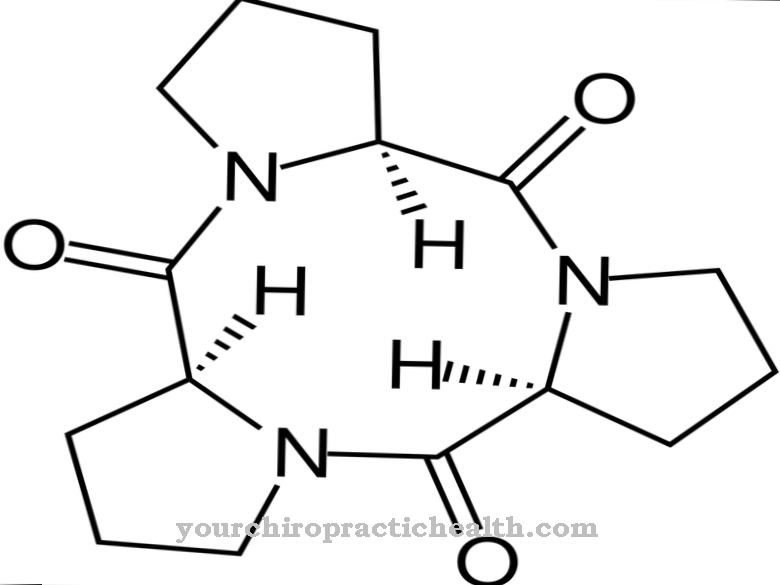
The body synthesizes the various opsonins in different organs. For example, the liver makes CRP. A single opsonin can consist of several hundred amino acids that combine to form a long chain. The sequence of the amino acids within the chain is determined by the genetic code. Mutations can disrupt the sequence of the amino acids and thereby change the structure of the opsonins. Possible consequences are diseases of the immune system, autoinflammatory diseases or disorders in the synthesis of the tissue.
Doctors can detect some opsonins by doing blood tests. The check can, for example, help to uncover an invisible inflammatory reaction. The reference value for CRP is 10 mg / l for a healthy adult. If the measured value is higher, this is an indication of an acute infection or inflammatory reaction. Further examinations or other blood parameters such as disease-specific inflammation markers can possibly provide the exact cause of abnormal opsonin values.
Diseases & Disorders
The individual opsonins can be related to diseases in different ways. A mutation in the FN1 gene changes the opsonin fibronectin, which promotes the binding of phagocytes to antigens. As a result, the X-type of Ehlers-Danlos syndrome can manifest itself.
The clinical picture is characterized by a disorder of the connective tissue. Above all, the overmobility of the joints and the overstretchability of the skin are characteristic. In addition, Ehlers-Danlos syndrome leads to changes in muscles, vessels, internal organs, tendons and ligaments. Since the syndrome affects numerous organ systems, the symptoms are very diverse: They include heart problems, early osteoarthritis, degeneration of the intervertebral discs, soft and thin skin, frequent injuries, delayed motor development in children, abnormalities in the teeth and gums, slight or severe digestive disorders, neuralgia , Migraines, eye diseases and many other ailments and disorders.
In addition, psychological symptoms such as unusual anxiety, depression, pain and sleep disorders often manifest themselves. To diagnose Ehlers-Danlos syndrome, doctors need to consider the clinical picture and also find out whether family members have the rare disease. Although they normally work for the benefit of health, the complement factors can cause direct damage to the human organism - if they get out of control and damage the body's own tissue. This process occurs, among other things, in rheumatoid arthritis or systemic lupus erythematosus.
The opsonin PTX3 appears to be involved in the immune response in various circumstances. For example, it reacts to the influenza virus, appears more frequently in cases of kidney failure and supports the defense against a fungal infection by Aspergillus fumigatus. Furthermore, PTX3 is also involved in the inflammatory response in rheumatoid arthritis, SIRS, sepsis and others.