As Papillitis is a subtype of optic nerve inflammation in which the optic nerve is damaged in its course on the so-called optic nerve head (papilla). Papillitis causes visual disturbances up to and including complete loss of vision.
What is papillitis?

© elvira fair - stock.adobe.com
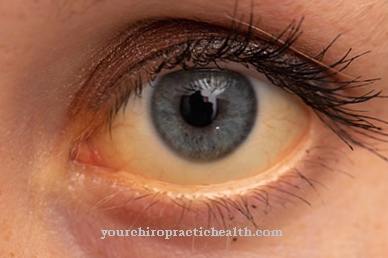
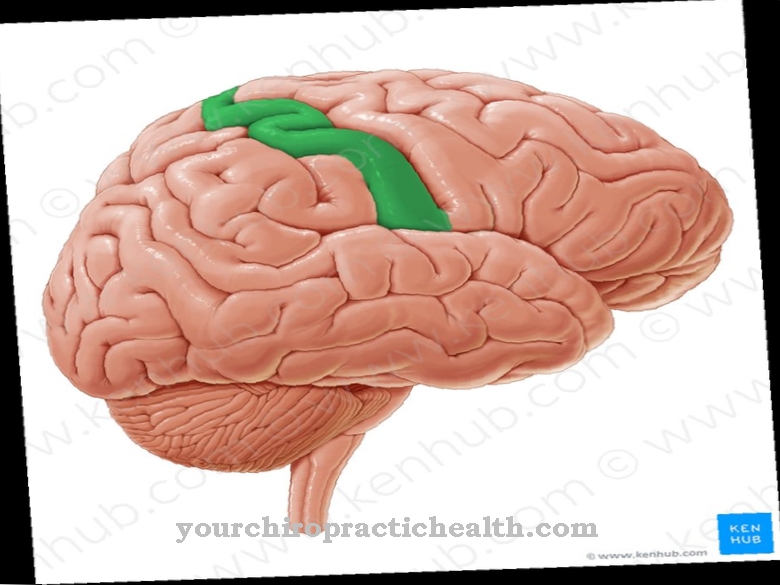
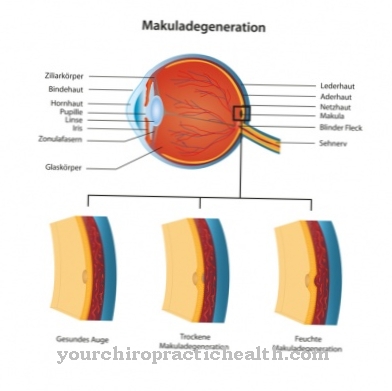
In optic nerve inflammation, a distinction is made between different subspecies depending on the localization of the inflammation. From one Papillitis one speaks when the diseased part of the optic nerve is located in the eye. The inflammatory reactions manifest themselves in the optic nerve head - the point where the nerve cords of the inner retinal layer bundle and emerge from the eye as the optic nerve. The optic nerve is responsible for transmitting the visual information signals to the brain.
The inflammation-related slowdown in the transmission of information therefore leads to a reduction in vision. The inflammation can also cause permanent damage to the optic nerve. The highest incidence of papillitis is in adults between 20 and 50 years. Statistically, however, women get sick more often than men.
causes
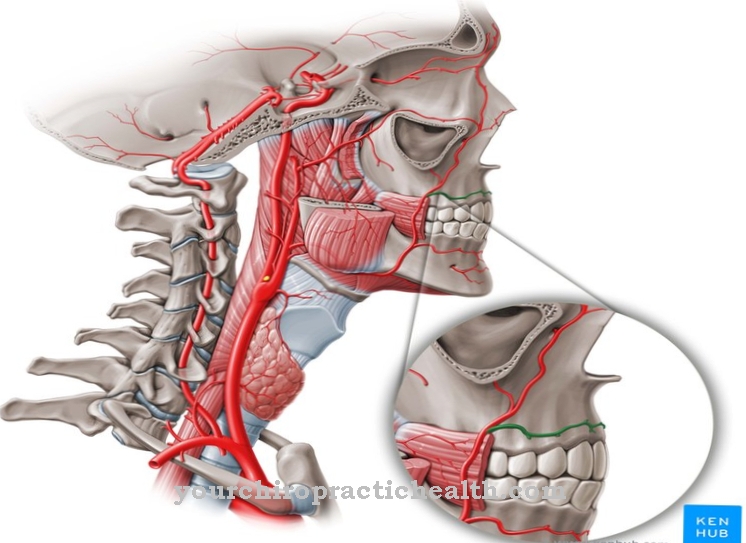
What exactly triggers the inflammation in the optic nerve head cannot be clearly explained in the majority of cases. Papillitis can be attributed to inflammatory diseases, allergies and autoimmune diseases, but also to infections or poisoning. The spread of a focus of inflammation from neighboring anatomical structures such as the eye socket, paranasal sinuses or the base of the skull can lead to papillitis.
In children, inflammation of the optic nerve head usually occurs in connection with an infection of the upper airways. In adults, however, usually in connection with inflammation of the vessel walls (vasculitis) or the brain (encephalitis). Bacterial and viral infections (such as spotted fever, syphilis, malaria and diphtheria) can also cause inflammation of the papilla.
Autoimmune diseases such as Crohn's disease, Wegener's disease or lupus erythematosus are also considered to be triggers. Other causes include metabolic diseases (e.g. diabetes mellitus) and poisoning with methanol, quinine or heavy metals.
Symptoms, ailments & signs
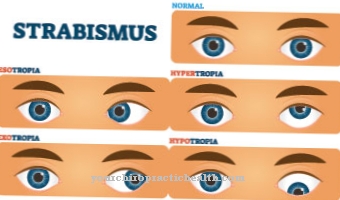
Typical symptoms of papillitis are acute visual disturbances. Those affected have reduced visual acuity and a reduced perception of colors and contrasts. Central visual field deficits (central scotoma) are also possible. With this quasi-blindness, the space visually captured by the immobile eye appears in the middle as a black-gray spot.
Usually only one of the two eyes is affected by the inflammation and the associated visual impairment. In addition, patients complain of a painful feeling of pressure in the back of the eyeball. The inflammatory processes can also spread to the motor nerves, which leads to pain when moving the eyes.
There can also be painful sensitivity to pressure and light. The spread of the inflammatory pain can also trigger deep headaches. Symptoms can be made worse by increased body temperature as a result of hot baths, saunas, or exercise.
Diagnosis & course of disease
The course of the disease of papillitis are different. Typically, as the inflammation heals, symptoms decrease. Despite accelerating the healing process with medication, several weeks or months can pass before symptoms are free. Serious inflammation, on the other hand, can lead to permanent visual defects or blindness of the affected eye due to the permanent damage to the optic nerve head.
The diagnosis of optic nerve inflammation is generally difficult. The patient's medical history is clarified beforehand based on the patient's medical history. The affected eye is inspected during the clinical examination. The sensitivity to pain can be tested by manually exerting pressure on the eyeball. During the ophthalmoscopic examination with the ophthalmoscope, a slightly swollen, blurred and reddened optic nerve head can be seen.
The pupil reaction can be determined using the alternating exposure test. Due to the inflammation, the pupillary reflex of the affected eye is sluggish, which shows up in a noticeably dilated pupil. In addition, a failure of the central field of view can be determined as part of the visual field measurement (perimetry).
By deriving visually evoked potentials (VEP), the optic nerve is also assessed. With papillitis, a delayed nerve conduction velocity is revealed. Imaging procedures such as magnetic resonance imaging (MRT) or computed tomography (CT) are available for further diagnosis.
Complications
A variety of causative factors can be responsible for inflammation of the bundled optic nerves at their exit point from the eyeball, the papilla. The exact cause of papillitis, as the inflammation of the nerves is called, is not always recognized. The main causes are infections and foci of inflammation in nearby tissues, poisoning, allergies or autoimmune reactions of the immune system. Metabolic diseases such as diabetes mellitus can also trigger papillitis.
Complications that arise in the context of papillitis are central visual field defects, which, if the underlying disease is not treated, can lead to blindness in the affected eye. In those cases in which the underlying disease heals without treatment, the complications of papillitis also resolve themselves without treatment.
There is a particular focus on causative factors such as diabetes mellitus and autoimmune diseases that worsen if left untreated. For example, it is of enormous importance in type 2 or 1 diabetes that the blood sugar level is well controlled and controlled in order to avoid papillitis and damage to the vascular wall of the arteries and arterioles.
To avoid further complications, the course of autoimmune diseases is also important for targeted therapeutic measures.For example, the breakdown of the myelin sheaths of the bundled optic nerves due to an autoimmune disease is not reversible in the advanced stage, so that in this case no complete restoration of vision is possible.
When should you go to the doctor?
Loss of vision is fundamentally a cause for concern. If they persist despite a recovery phase or a good night's sleep, a doctor should be consulted. In many cases, decreased vision can be triggered due to overwork or overexertion. Here, after sufficient rest and protection, there is complete regeneration of the usual vision.
In the event of acute loss of vision, a doctor should be consulted immediately. Reduced visual acuity as well as reduced perception of contours or colors should be presented to a doctor. If a black or gray spot can be noticed in the field of vision, this is considered a sign of illness.
If pain occurs as soon as the eyes are moved, a doctor should be consulted. Sensitivity to light stimuli or slight pressure exerted on the eye should be examined and treated. A doctor is also required in the event of headaches, an increased risk of falls or accidents or psychological irregularities.
Papillitis is characterized by an increase in symptoms as soon as sporting activities take place or the person concerned is in an environment with an increased ambient temperature. A sudden inability to see in a sauna or hot bath should therefore be brought to a doctor immediately. If the behavior shows aggressive tendencies or tearfulness, clarification of the cause is required.
Therapy & Treatment
The treatment of papillitis is based on the trigger of the inflammatory process. Depending on the cause or the underlying primary disease, neurological or internal measures may be taken. Drug therapy with anti-inflammatory corticosteroids (e.g. cortisone) accelerates the resolution of the inflammation and is often indispensable for the prevention of long-term damage if the inflammation is severe.
For high-dose, drug treatment with corticosteroids, however, no other diseases such as tuberculosis, stomach ulcers, diabetes mellitus or high blood pressure must be present. The anti-inflammatory drugs are administered orally, but can also be administered intravenously in the context of high dosages and for faster effectiveness. The intake of cortisone can have side effects and is therefore not without risk depending on the underlying disease.
Side effects include weight gain, osteoporosis, water retention, and a weakened immune system. If the cause of the papillitis is determined to be infectious, the relevant pathogen is treated with antibiotics or antivirals. In general, the chances of recovery are good if the causes and symptoms of the inflammation are treated quickly. If therapy is initiated with a delay, however, longer-lasting inflammation, greater complications and, ultimately, a poorer prognosis can be expected.
You can find your medication here
➔ Medicines for visual disturbances and eye complaintsOutlook & forecast
Papillitis offers a relatively good prognosis. Eyesight often deteriorates gradually, often as a result of an infection, and gets worse within a week or two before the disease bottomed out. With early therapy, the inflammation of the optic nerve subsides within four to five weeks. However, many patients report persistent problems seeing colors and contrasts. The atypical forms often leave severe visual problems.
If the papillitis remains untreated, the optic nerve papilla can be lost. If the optic nerve papilla disappears, eyesight remains severely restricted. The prospect of recovery is therefore only given with early treatment. Due to poor eyesight, patients' quality of life is limited during the illness. In contrast, life expectancy is not reduced. However, papillitis is often linked to multiple sclerosis, which usually takes a severe course and is associated with other health complications.
The prognosis of papillitis is made by the ophthalmologist or a neurologist. The prognosis is based not only on the time of diagnosis, but also on the general condition of the patient and the willingness to use various therapy methods.
prevention
Since the triggers of papillitis remain unexplained in most cases, there is no clearly identifiable, effective preventive measure. However, regular ophthalmological check-ups are advisable for the corresponding underlying illnesses.
Aftercare
In most cases, the affected person has only limited direct follow-up measures available. For this reason, early diagnosis of this disease is very important so that further complications can be prevented. The papillitis cannot heal itself, so that the person affected can completely lose sight if the disease is not treated in time.
Most patients are dependent on the intake of various medications that can alleviate and limit the symptoms. The person concerned should always pay attention to the correct dosage and regular intake of the medication in order to relieve the symptoms permanently and correctly. When taking antibiotics, it should also be noted that they must not be taken together with alcohol.
Regular checks and examinations by a doctor are also very important and can prevent further complications. A direct prediction of the further course of papillitis is usually not possible, as this depends heavily on the time of diagnosis and the severity of the symptoms. In some cases, this disease also reduces the life expectancy of those affected.
You can do that yourself
Papillitis is usually treated with the help of cortisone. The patient can support the cortisone therapy by keeping close consultation with the doctor during the therapy and informing him of any accompanying symptoms. Close monitoring is particularly important when administering high doses of cortisone, as there is an increased risk of side effects and interactions.
In addition, it is important to protect your eyes. Direct sunlight should be avoided as well as contact with aggressive care products. Patients should get enough sleep and avoid stress. If necessary, the diet must be changed temporarily. Bland foods support the immune system and help fight the causative pathogen. If the papillitis is caused by an autoimmune disease, further changes must be made. The doctor in charge will usually give the patient the necessary tips and can call in other specialists if necessary.
If, despite all measures, problems arise again, the doctor must be informed. In the case of serious illnesses, all self-help measures should be discussed with the doctor beforehand. The use of alternative remedies is best done in consultation with a specialist.



.jpg)
.jpg)

.jpg)