The paroxysmal nocturnal hemoglobinuria (PNH) is a rare and serious disease of hematopoietic cells that is genetic, but only acquired later in life. Since it is a somatic mutation, the germ cells are not affected. If left untreated, the disease can be fatal, mainly through the development of multiple thromboses.
What is paroxysmal nocturnal hemoglobinuria?

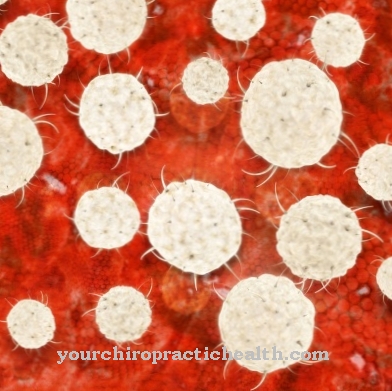
© blueringmedia - stock.adobe.com
The paroxysmal nocturnal hemoglobinuria is an often difficult disease of the blood-forming cells. It is characterized by hemolysis, thrombus formation and a reduced formation of blood cells. Individual or all blood line cells can be affected.
While all patients with PNH show the symptoms of hemolysis, the other symptoms are very variable. Fatal outcome can occur in around 35 percent of cases, which is mainly caused by the large number of thromboses that occur. The constant hemolysis results in chronic anemia, which is accompanied by severe states of exhaustion.
Although the disease cannot be cured, it can be managed well therapeutically. With lifelong consistent treatment, a good quality of life is achieved with normal life expectancy. PNH has an estimated prevalence of around 16 per 1 million population and is therefore one of the very rare diseases.
causes
Paroxysmal nocturnal hemoglobinuria is caused by a somatic mutation of the PIG-A gene. This gene is located on the X chromosome and is responsible for coding the enzyme N-acetylglucosaminyltransferase. N-acetylglucosaminyltransferase catalyzes the formation of the so-called glucosylphosphatidylinositol anchor (GPI anchor), which ensures that protective proteins are anchored on the cell surface of the blood cells.
These include the proteins CD55 and CD59. With their anchoring on the cell membrane of the blood-forming cells, they serve to protect them from attack by the part of the immune system known as the complement system. If these anchor proteins are not present, blood-forming stem cells and blood cells are destroyed
In addition to increased hemolysis, fewer blood cells are also formed. There is pronounced chronic anemia. At the same time, thromboses occur in many parts of the body, which can be dangerous. PNH is an acquired disease that occurs for the first time, especially between the ages of 25 and 45.
The underlying gene mutation has not been present since birth. It arises from a somatic mutation of the PIG-A gene within the multipotent hematopoietic stem cells. Otherwise no cases of PNH are found in the family or relatives. Since the germ cells are not affected, this disease cannot be passed on to offspring.
Symptoms, ailments & signs
The main symptom of paroxysmal nocturnal hemoglobinuria is chronic hemolysis. Due to the somatic mutation, so-called mosaics are present. There are both healthy and defective blood cells. All mutated blood cells have lost protection from the complement system due to the missing anchor and are destroyed.
The diseased erythrocytes are particularly affected. However, the most dangerous symptom is the propensity for thrombosis in both the venous and arterial systems. This is the case in around 50 percent of patients with PNH. The thrombosis is also responsible for most of the deaths, affecting a third of those affected.
Further symptoms are severe exhaustion (fatigue), abdominal cramps, headache, swallowing disorders, nausea, chest pain, back pain or erectile dysfunction. The pain is caused by small thrombi. They can be mild or so strong that opiates even have to be administered as pain relievers.
The pain is also explained by the lack of nitric oxide (NO), which binds to released hemoglobin. Since NO is responsible for the relaxation of the smooth muscles, the lack of NO leads to increased levels of tension there. The severity of the disease also depends on how many bloodlines are affected by the mutation. If the immune cells of the blood are mutated at the same time, the immune system is also severely weakened.
Diagnosis & course of disease
During the diagnosis, the blood cells are examined for the presence of protective proteins using flow cytometry. This method can be used to identify the cells that lack protection from the complement system. A clear diagnosis is made when at least two cell lines such as erythrocytes or granulocytes do not have a protective factor.
Complications
In the worst case, this disease can lead to death of the person concerned. As a rule, however, this only occurs when the person concerned suffers from multiple thromboses that were not prevented. The risk of developing thromboses is significantly increased in the patient. In most cases, these are also responsible for the patient's death.
Those affected suffer from pain that occurs in different places. This leads to pain in the head or in the stomach. In many cases, there is also chest pain that can spread to the back. Men can also suffer from erectile dysfunction due to the disease. Furthermore, there is permanent nausea or difficulty swallowing. In many cases, ordinary pain relievers are no longer sufficient to relieve the pain.
The quality of life of those affected is significantly reduced by the disease. The treatment takes place without complications. With the help of blood transfusions or a stem cell transplant, the symptoms can be reduced. However, the life expectancy of the patient is usually reduced due to illness.
When should you go to the doctor?
This disease must always be examined and treated by a doctor. Without treatment, death usually occurs as the disease leads to the development of thrombosis. Those affected suffer from various ailments that do not always point directly to the disease. Pain in the head or stomach can occur, which is accompanied by nausea or back pain. A potency disorder can often indicate this disease. If the symptoms persist and do not go away on their own, a visit to a doctor is definitely necessary.
The pain can also be so extreme that the person affected may lose consciousness. A weakened immune system can also indicate this disease. If you have frequent colds or other infections, you should also consult a doctor. The first diagnosis of the disease can be made by the general practitioner. However, a specialist is required for further treatments. Whether the disease will lead to a reduced life expectancy cannot generally be predicted.
Treatment & Therapy
There is no cure for PNH. However, there are some supportive treatments that can improve the quality of life. First of all, due to the chronic anemia, regular blood transfusions or transfusions of red cell concentrates are necessary. Folic acid or vitamin B12 are recommended to promote blood formation.
Infections must be detected early and treated with antibiotics because they can trigger hemolytic crises. Short-term use of steroids can alleviate a hemolytic crisis. However, steroids must not be given permanently. Severe pain requires treatment with pain relievers.
If a thrombosis has occurred, coumarins are given permanently as an anticoagulant. The only real possibility of curing paroxysmal nocturnal hemoglobinuria is a stem cell transplant. However, it is associated with considerable risks, so that this therapy is only considered in very severe cases.
Good experiences have been made with the drug eculizumab. These are genetically engineered monoclonal antibodies that inactivate the complement factor C5 of the complement system. This prevents the attack on the unprotected blood cells.
Outlook & forecast
In paroxysmal nocturnal hemoglobinuria, a prognosis is difficult. The clinical picture of this acquired hematological disease can be very different. The prognosis is more positive for milder forms. In the case of severe stem cell damage, a stem cell transplant is often the only way to prolong life. Since the disease is based on a genetic mutation in the bone marrow, there is no cure for it.
Paroxysmal nocturnal hemoglobinuria can only be treated symptomatically. A distinction is made between treatment for symptomatic and asymptomatic courses. Patients with asymptomatic paroxysmal nocturnal hemoglobinuria are given prophylactic anticoagulant drugs. In symptomatic patients, therapy with an antibody called eculizmab, in conjunction with other supportive measures, can reduce symptoms.
The bone marrow transplant is another treatment option. However, it is fraught with high risks because the immune system must be switched off before the transplant. In the end, the severity of the stem cell changes determines how good or bad the prognosis is. Half of those affected only survive the diagnosis by 15 years.
In the past, the prognosis for paroxysmal nocturnal hemoglobinuria was worse than it is today. Modern treatment methods have significantly improved the prognosis for the symptomatic type of disease. Nevertheless, it cannot be called good. The survival time and quality of life of those affected are better today than they used to be.
prevention
Prevention of paroxysmal nocturnal hemoglobinuria is not possible. However, people who are already ill should protect themselves from infections so as not to trigger a hemolytic crisis. Long-term therapy with eculizumab prevents the symptoms of PNH and enables normal life expectancy.
Aftercare
Since paroxysmal nocturnal hemoglobinuria is a genetic disease, there are currently no causal treatment options. If the affected patients are asymptomatic, one should first wait or refrain from therapy. Only oral anticoagulation can be considered prophylactically.
The coagulation parameters must be constantly monitored. Follow-up care therefore refers to the control and monitoring of supportive therapies against the multiple symptoms of the disease. Long-term monitoring of the blood values for VitB12 and folic acid are indicated in order to prevent changes in the blood components and the resulting symptoms. These deficiencies in VitB12 or folic acid can then be substituted with medication.
Regular blood counts are necessary in order to detect any infections at an early stage. If glucocorticoids are administered, multiple treatment monitoring measures should be taken. Since long-term use of cortisone can lead to decalcification of the bones, this promotes the development of osteoporosis. Calcium and VitD should be administered prophylactically.
Since blood sugar levels and blood pressure rises can also occur in the course of therapy, these parameters are also checked regularly. If treatment with oral anticoagulation is used, regular coagulation parameters will be checked. When taking coumarin, it is essential to watch out for pharmacokinetic interactions with other drugs. Even with therapy with monoclonal antibodies, the occurrence of side effects must always be observed in order to intervene medically if necessary.
You can do that yourself
Since the disease is based on a genetic defect, relatives of a patient should initiate a control of their genetic predispositions independently and independently.
Since thrombosis is more likely to occur if people remain in a rigid posture for too long, the musculoskeletal system must be checked. Avoid standing, squatting or sitting for long periods of time. In addition, the circulatory system should be supported in everyday life through various relaxation exercises. In this way, blood congestion can be avoided and vessels in the organism are not pinched.
Do not consume harmful substances such as nicotine or medications that have side effects on the blood system. In the case of an existing illness, the preparations taken should be checked for their risks and consultation with the treating doctor should take place. In some cases a change in the treatment plan is necessary. If exhaustion, tiredness or an increased need for sleep occur, the person concerned should react sufficiently to the signals from his body. The organism should not be excessively stressed, as sequelae or complications threaten.
Changes in the feeling of health or an increase in symptoms should be discussed with a doctor immediately. Paroxysmal nocturnal hemoglobinuria, if left untreated, can lead to a life-threatening condition. Therefore, if the self-help measures are not effective enough, consultation with a doctor is essential.









.jpg)



.jpg)










.jpg)
