In the context of diseases of the cardiovascular system, very different clinical pictures occur, which not only affect the heart, but also the blood vessels and the organs involved. This also includes the peripheral arterial disease, short PAOD.
What is Peripheral Arterial Disease?

The peripheral arterial disease is also called in medicine PAOD Abbreviated and based on a predominantly mechanical impairment of the unimpeded flow of blood through the arteries.
Peripheral arterial occlusive disease is so named because, over time, the arteries can block, causing an interruption in blood flow. PAD is therefore one of the life-threatening health impairments that are predominantly limited to the lower extremities.
Peripheral arterial occlusive disease in the arms is rare. In colloquial usage, peripheral arterial occlusive disease is often referred to as intermittent claudication, which can be recognized by very typical symptoms and can enormously limit the quality of life of those affected.
causes
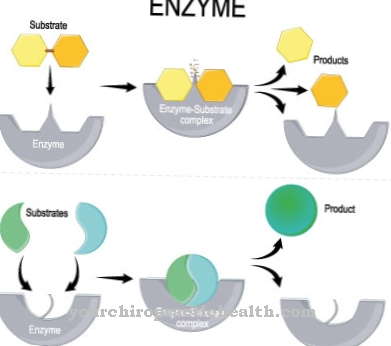
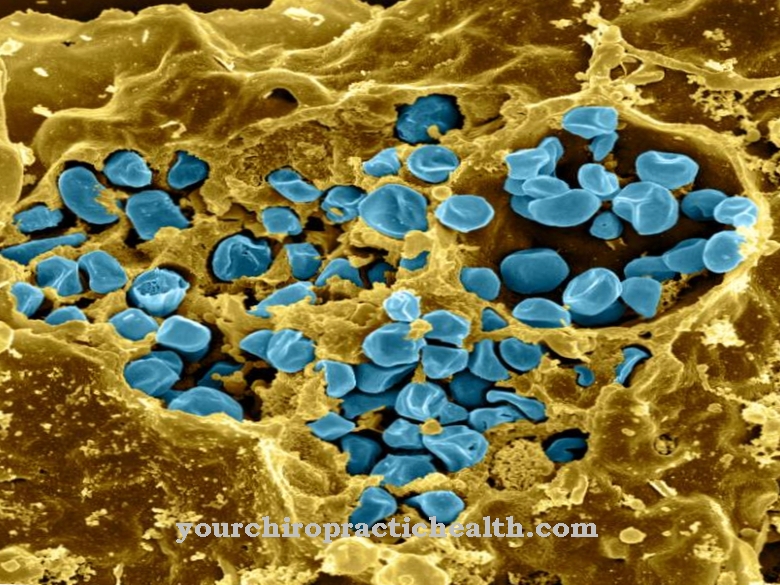
A typical reason why a peripheral arterial disease can develop is an existing arteriosclerosis, within which the blood vessels become clogged by solid micro-deposits. In this context, arteriosclerosis not only occurs in the venous and capillary vessels, but is also considered a direct trigger for PAD.
The primary causes and risks that can trigger peripheral arterial occlusive disease include the same factors that are also relevant for arteriosclerosis.
In addition to the consumption of nicotine and alcohol, these are also various previous illnesses such as high blood pressure, diabetes mellitus and obesity, which is associated with a high cholesterol and fat content in the blood. A lack of exercise and individual hereditary factors also play a role in peripheral arterial occlusive disease.
Symptoms, ailments & signs
The disease is divided into four stages. At the beginning, in stage I, the symptoms are still absent. Although the vessels are gradually constricting, the person concerned is not yet able to feel anything. In the absence of symptoms, the disease is usually not yet discovered at this point, even if it could already be diagnosed with an appropriate examination.
In stage II, the first pain in the legs can be felt, whenever the patient has walked a distance of about 200 meters. He has to stop and wait again and again, because when he stands his legs stop hurting. This is known as stress-related pain. If stage III is reached, legs ache even at rest.
Regardless of whether the person is lying down or sitting, the muscles hurt. Walking is almost impossible or only possible with pain. In stage IV, the skin begins to change because the tissue is no longer supplied with enough oxygen due to the reduced blood flow. Ulcers develop on the heels and toes and, as the disease progresses, the tissue dies. It turns black and starts to rot. If this necrosis continues, amputation of the leg may be necessary.
Diagnosis & course
The complaints caused by peripheral arterial disease noticeably triggered for those affected, consist of pain, general physical weakness and weakness.
In addition, people who suffer from PAD have pale skin and often suffer from cold feet. Pain is usually felt in the legs due to peripheral arterial occlusive disease and is primarily localized in the calf muscles. For this reason, patients with PAD have to stand still while walking and it seems as if they are looking at the shop window.
This abnormality occurs due to peripheral arterial occlusive disease only when the advanced stage has already been reached. The PAD can be precisely identified with a basic diagnosis and a subsequent differential diagnosis.
Complications
The development and course of peripheral arterial occlusive disease (PAD) is favored by several factors. In principle, it is an arteriosclerosis that leads to circulatory disorders and causes consequential damage, especially in the legs - to a much lesser extent also in the arms. If the causative factors that led to the development of arteriosclerosis are not eliminated, further complications will arise in addition to severe and sometimes cramp-like pain in the calves and the other leg and gluteal muscles.
Local complications can be open, poorly healing wounds, with partially necrotizing tissue and further progressive stenoses in the corresponding arteries. If left untreated, PAD can even require amputation as the last treatment step in its advanced stage. The other complications can also be independent of local effects of the affected arteries of the extremities, because the underlying disease, arteriosclerosis, can also extend to other arteries and to the coronary arteries.
As a result, the risk of suffering a heart attack or stroke increases dramatically. In order to be able to limit the risk of a stroke, an examination of the carotid arteries (arteria carotis) is recommended for arteriosclerotic changes that arise due to plaques. If the PAD is detected at an early stage and the causes of the arteriosclerotic changes can be successfully eliminated, there is a chance that the symptoms will regress and a return to a symptom-free life is possible.
When should you go to the doctor?
A doctor should be consulted at the first signs of peripheral arterial occlusive disease. If circulatory disorders, dizziness, and other unusual symptoms are noticed, it suggests a condition that needs clarification. From the age of 35, blood pressure and blood lipid values should be measured regularly. People with statutory and private health insurance can take advantage of the so-called “Check-up 35”. The check-up should then be carried out every two years, because in this way cardiovascular diseases, kidney diseases and diabetes can be detected at an early stage.
Peripheral arterial disease primarily affects people who lead an unhealthy lifestyle, are alcoholic, overweight, or have a genetic predisposition. Whoever these risk factors apply to should consult their family doctor as soon as possible. Ideally, the triggers are corrected before peripheral arterial disease can develop. In addition to the family doctor, an internist or a cardiologist can be consulted. Depending on the cause, physiotherapists, nutritionists, alternative medicine specialists and therapeutic specialists are involved in the therapy.
Treatment & Therapy
The therapy that is successful peripheral arterial disease can heal is extremely extensive, as the PAD can be divided into several degrees of severity. In addition, with every degree of severity of peripheral arterial occlusive disease, various complaints and risks are associated, the reduction of which is largely important.
In order to be able to treat the PAD in a targeted manner, several therapy methods are required in combination. These relate to quitting nicotine consumption and reducing physical obesity, as well as a healthy, balanced diet paired with regular exercise. With peripheral arterial occlusive disease, it is important to lower cholesterol and high blood pressure and to improve the blood flow in the arteries again.
In order to prevent a heart attack or stroke caused by PAD, medical procedures as well as so-called interventional and surgical techniques are carried out. In interventional procedures for the therapy of arterial occlusive disease, the affected sections of the arteries are widened with a surgical balloon or the nerve conduction is interrupted.
You can find your medication here
➔ Medicines for smoking cessationOutlook & forecast
The prognosis for peripheral arterial occlusive disease depends on successful treatment of the underlying causes. If treatment fails or is unsuccessful, the serious illness takes its course unhindered. However, it is entirely possible to make the prognosis more positive if the patient is striving for a healthier lifestyle. It includes a balanced diet, avoiding tobacco products, reducing excess weight and regular exercise.
The achievement of normal values for blood pressure, blood lipid values and blood sugar also has a positive effect on the course of PAD. If the patient also suffers from illnesses such as diabetes mellitus or high blood pressure, it is important to treat them specifically and consistently.
Basically, the life expectancy of people who suffer from peripheral arterial occlusive disease is classified as lower. The reason for this are the vascular diseases that also occur.
As a rule, the prospects of the disease also depend on the point in time between the first appearance of symptoms and a successful vascular reopening. If the period in the event of an arterial blockage in the leg is less than six hours, the leg can be preserved in 96 percent of all patients. However, if more than 12 hours pass, around 40 percent of all those affected have to be amputated. In the case of an acute artery occlusion, the survival rate of those affected after surgery is around 80 percent.
prevention
For the prevention of a peripheral arterial disease the elimination of all risk factors that favor high blood pressure, obesity and diabetes mellitus is beneficial. If these diseases are already present, optimal treatment should be given.
Regular checks and adjustments of blood sugar levels are also important. Nicotine consumption and too little physical exercise as well as a permanent excess of stress should be switched off as far as possible when it comes to taking preventive action against PAD. This is the only way to achieve a long life expectancy with top performance.
Aftercare
Follow-up care for peripheral arterial disease is extremely important. Its aim is to keep the arteries open. Renewed narrowing or the formation of blood clots should be avoided at all costs. Another goal of follow-up treatment is to improve or maintain the quality of life. The aim is to reduce the risk of a stroke or heart attack.
One of the most sensible measures of PAD follow-up care is regular check-ups. This applies regardless of catheter treatment, surgery or medication. The follow-up examinations take place at the family doctor and a vascular specialist. Together with the family doctor, they are working on a healthier way of life, which primarily includes sufficient exercise, a healthy diet and avoidance of nicotine.
The doctor will also check your blood pressure, weight and cholesterol levels at regular intervals. Ideally, the vascular monitoring program lasts at least two years. In principle, all PAOD patients must have a medical check-up for the rest of their lives. To support the follow-up treatment, it is advisable to complete a gait training session. It is advisable to do it in a vascular exercise group.
The vascular specialist checks the ABI value both after exercise and at rest. The doctor also uses duplex sonography to check the condition of the blood vessels. Medications that are administered during PAD follow-up treatment are platelet function inhibitors such as clopidogrel or acetylsalicylic acid. They are mostly used during the main treatment.
You can do that yourself
Coping with everyday life and self-help options depend on the severity of the peripheral arterial occlusive disease (PAD). In stages I and II, in which there is only a slight impairment or in which walking distances of up to 200 m can be managed relatively easily, self-help measures are mainly aimed at combating the causes of PAD.
For example, if you are a smoker, stopping smoking, if you have diabetes a good adjustment of the sugar values and in hypertensive patients a good adjustment of the blood pressure can lead to a significant improvement in symptoms. Significant overweight is also one of the risk factors that favor PAD. In addition, regular physical activity has a positive effect on PAD as far as possible. A regular extra portion of omega-3 fatty acids has a positive effect. For example, a single tablespoon of cold-pressed linseed oil per day can help reduce the arterial inflammatory processes that are ultimately the cause of arterial constrictions in the extremities. A low ratio of omega-6 to omega-3 fatty acids of around 2: 1 to a maximum of 5: 1 is important in order to combat arterial inflammatory processes with natural means.
The extent to which increased cholesterol levels, in particular increased LDL concentrations with a simultaneously reduced HDL fraction, play an essential role as causative factors for PAD is controversial. A ratio of LDL to HDL below 3.5 is considered to be beneficial for health with an anti-inflammatory effect on the arteries.


.jpg)
.jpg)












.jpg)