Plasmodium malariae is a parasite belonging to the genus Plasmodia. The protozoa is the causative agent of the infectious disease malaria.
What is Plasmodium malariae?
Plasmodium malariae is a protozoan that is classified as a parasite. This means that the Plasmodium lives at the expense of the host. In addition to Plasmodium falciparum, Plasmodium ovale and Plasmodium vivax, Plasmodium malariae is one of the causative agents of malaria. The single cell causes quartana malaria. This form of malaria is comparatively benign and rarely has a fatal outcome.
The malaria pathogen was first described in 1880 by the French physician Alphonse Laveran. But it was not until 1954 that the common name combination Plasmodium malariae was introduced by the International Commission for Zoological Nomenclature.
Occurrence, Distribution & Properties
Towards the end of the Second World War, malaria spread to northern Europe and North America. Today the infectious disease is typical of the tropics. It occurs mainly in subtropical and tropical areas. Malaria is endemic in all continents with the exception of Australia. Around 200 million people fall ill every year. 600,000 of them die of the disease.
The main distribution areas of Plasmodium malariae are in Africa, Asia and South America. The pathogen is not widespread in Germany. However, around 500 to 600 cases of malaria are imported each year. However, the proportion of infections caused by Plasmodium malariae is just under 10 percent.
Most experts regard humans as the only reservoir host for the pathogen. However, infected monkeys may also represent a reservoir.
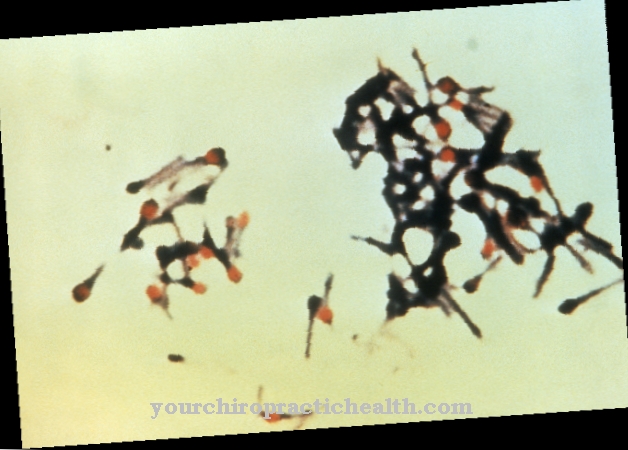
Plasmodium malariae is transmitted by the anopheles mosquito. In the mosquito, the pathogen is in the developmental stage of the sporozoites. These have a diameter of 12 micrometers and enter the human bloodstream through a bite from the infected mosquito. From there they migrate to the liver and penetrate the liver cells.
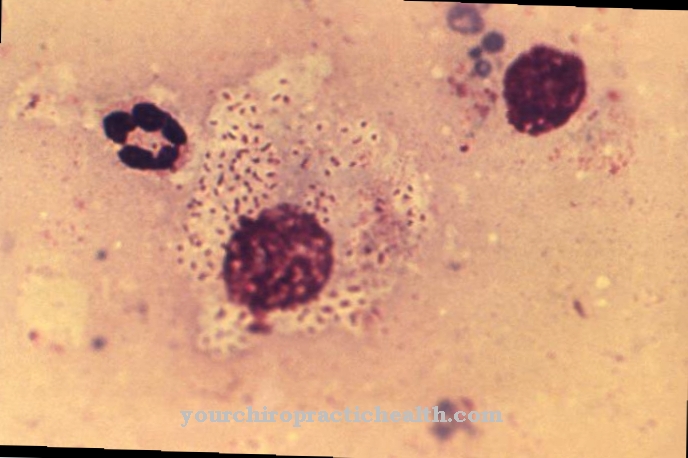
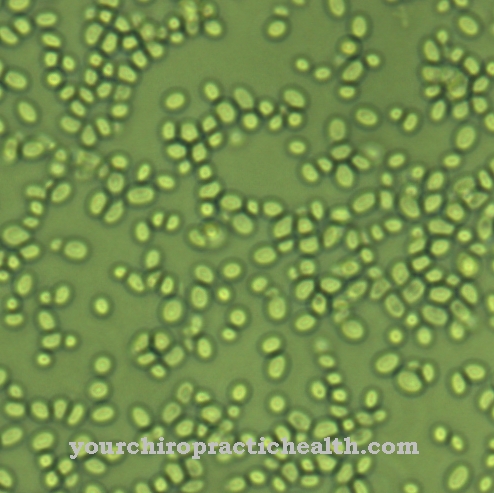
There the sporozoites can reproduce asexually. The incubation period for this liver phase is around two weeks. The so-called liver schizonts produce many merozoites. These are released and affect the red blood cells. They reproduce asexually in the blood cells. At the end of the 72-hour reproduction cycle, many new parasites are released, which are washed into the bloodstream and infect red blood cells again.
Only some of the plasmodia develop into sexual forms in the red blood cells. These sex forms are called microgametocytes or macrogametocytes. They are ingested by mosquitoes when they bite an infected person and continue to develop in the insect's intestines. New sporozoites form, which then migrate into the mosquito's salivary gland and can be transmitted from there to another person.
Illnesses & ailments
The infectious disease malaria, which is triggered by the pathogen Plasmodium malariae, begins with uncharacteristic symptoms such as fever, headache, muscle pain and a general feeling of illness. At this stage of the disease, the misdiagnosis of flu is often made.
Since the parasites are released into the blood every 72 hours, fever attacks occur every 72 hours. Chills typically develop in the late afternoon hours. Over time, the fever rises very quickly to values above 40 ° Celsius. After three to four hours, the temperature suddenly drops to normal. During this fall in fever, patients sweat profusely.
However, it should be noted that a lack of fever rhythm is not an exclusion criterion for the diagnosis of malaria. Quartana malaria can seriously damage the kidneys. This dangerous side effect is called malaria nephrosis. From a medical point of view, it is a nephrotic syndrome. This goes hand in hand with a reduced serum protein.
The serum proteins, also called albumins, regulate the water balance in the bloodstream. If there is a lack of albumins, water can collect in the tissue (edema) and water can collect in the abdominal cavity (ascites). To compensate for the loss of serum protein, the serum cholesterol level rises. Malaria nephrosis occurs as a complication especially in children between the ages of two and ten years in tropical Africa.
In contrast to the other plasmodia, Plasmodium malariae constantly attacks the blood. However, this persistent parasite infestation is so low that it often cannot be detected with a microscope. Due to the parasitic load on the blood, recurrences can occur even after a long period of time without disease. There are malaria recurrences that occurred more than 50 years after the original infection.
The lack of microscopic evidence is a risk for transfusion medicine in the endemic areas. Even with donors who have tested negative for malaria, the malaria can also be transmitted if fresh blood is transmitted. Cooling the blood supplies, however, kills Plasmodium malariae. The recurrences can also usually be prevented with medication.
Quartana malaria must be treated as an inpatient. The drug of choice here is chloroquine. Since Plasmodium malariae does not develop hypnozoites in the liver, in contrast to the other forms of malaria, quartana malaria does not require subsequent treatment with primaquine.
Travelers visiting malaria endemic areas should consider exposure prophylaxis. Mosquito-proof rooms with air conditioning and flyscreens, sleeping under mosquito nets and wearing long-sleeved clothing can reduce the risk of infection. The use of so-called repellents has also proven to be helpful.





















.jpg)



