Of the Brachial plexus is a plexus of nerves that innervates the areas of shoulders, arms and chest wall as part of the peripheral nervous system with three main branches. The brachial plexus is composed of anterior spinal nerves of the lowest cervical vertebrae C5-C7 and the first thoracic vertebra Th1. A few nerve fibers are also involved, which originate from the 4th cervical vertebra (C4) and the 2nd thoracic vertebra (Th2).
What is the brachial plexus?
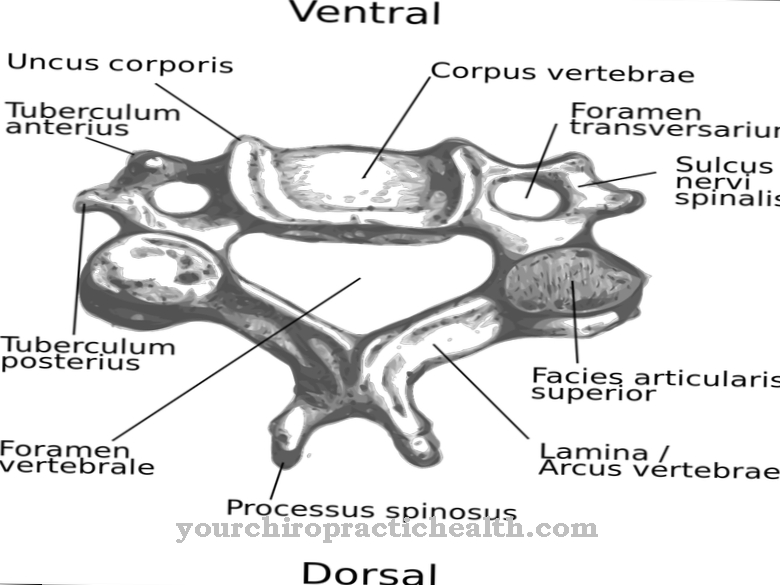
The Latin term plexus brachialis literally means “plexus of the arm”. It is a network of nerves in the peripheral nervous system, the main task of which is to innervate the muscles and skin areas of the chest, shoulders, arms and hands in a motor and sensory manner. The nerve plexus is formed by spinal nerves that originate from the lowest cervical vertebrae (C5-C7) and the uppermost thoracic vertebra (Th1) and are supplemented by a few nerve fibers from C4 and Th2.
The brachial plexus can be divided into the three areas of trunci (trunks), fasciculi (bundles) and the individual main nerves emerging from them. The spinal nerves emerging from the vertebrae partially branch when they enter one of the three trunks, so that it is not always possible to clearly differentiate or assign certain spinal nerves to one of the three main trunks. Further branches take place in the fasciculi, so that a kind of nervous network arises. The main nerves “responsible” for certain areas or muscles originate from the nerve plexus, and their origin goes back to several spinal nerves due to the networking within the brachial plexus.
Anatomy & structure
The brachial plexus is made up of the spinal nerves of the spinal area C5-Th1 emerging from the front between the vertebrae. In addition, the plexus takes on a few nerve fibers from C4 and Th2. The spinal nerves from C5 and C6 together form the main trunk superior trunk. The spinal nerve of the 7th cervical vertebra forms the main trunk Truncus medius and the union of the lowest cervical vertebrae with the first thoracic vertebra forms the Truncus inferior.
A part of the main trunk nerves is networked to form a further three sub-trunks (fasciculi), the lateral, medial and posterior fasciculus. The partial bundling of the spinal nerves has the advantage for the motor and sensory nerves emerging from the network that mostly nerve fibers from several spinal nerves are involved. In the area of the brachial plexus are the two neck muscles, the anterior scalenus muscle and the medius scalenus muscle. There is a gap between the two muscles, the posterior scalene gap, through which the nerves of the brachial plexus and the subclavian artery enter the axilla.
Function & tasks
The main task and function of the brachial plexus plexus is the motor and sensitive innervation of the chest and shoulder muscles as well as the arm and hand muscles. The partial networking and union of the spinal nerves in the brachial plexus has the advantage that in the event of a lesion of a single spinal nerve, its function can be taken over to a certain extent by other nerve fibers. In addition, a kind of communication between the nerves is possible with a certain exchange of information about the current muscle parameters. The nerves that arise from the plexus to supply “their” muscles are made up of mixed fibers.
Efferent fibers convey the information about muscle contraction from the corresponding movement center to the muscle or the muscle area. Afferent, sensory (sensitive) fibers transmit sensory impressions to the appropriate centers in the brain, where they are processed and possibly part of an automatic control loop. Muscle spindles serve as sensors, which "measure" the tension of muscle fibers and, in combination with the Golgi tendon organs, transmit the proprioceptive state. It can be very complex control loops that enable an automatic or semi-automatic sequence of movements. Nerve fibers that serve the autonomous - not subject to the will - control are an integral part of the nerves emanating from the brachial plexus.
Diseases
The most common occurrence of complaints or certain symptoms in connection with the brachial plexus is a narrowing of the posterior scalenus gap, which can lead to the development of a so-called scalenus syndrome. Symptoms of scalena syndrome are pain in the forearm on the little finger side and paresthesia that increase in the area when the forearm is drooping.
When the posterior scalena gap is narrowed, the oxygen supply to the tissue is generally impaired because the artery supplying it also runs through the scalena gap. The scalena syndrome is therefore often accompanied by a blue discoloration (cyanosis) of the tissue and by edema due to the lack of oxygen supply and due to the mechanical impairment of the blood flow. If the brachial plexus is completely torn off as a result of an accident, it comes to a total failure, to a complete paralysis of the muscles in the shoulder, chest, arms and hands. In the case of a partial lesion of certain branches of the brachial plexus, symptomatic motor and sensory deficits of the affected muscle parts occur.
Damage to the brachial plexus can also occur during the birth process if the birth canal is a little narrow for the baby. Tensile forces can cause tearing or avulsion injuries to the nerve plexus and thus birth-trauma plexus palsy. The paresis usually manifests itself in a paralysis of the affected arm. The damage often heals by itself, otherwise surgical measures should be considered within the first 9 months. The brachial plexus can become inflamed in a kind of autoimmune reaction and lead to neuralgic shoulder amyotrophy. The disease manifests itself through severe pain in the shoulder and paralysis of the shoulder and upper arm muscles.
You can find your medication here
➔ Medicines for paresthesia and circulatory disordersTypical & common nerve diseases
- Nerve pain
- Inflammation of the nerves
- Polyneuropathy
- epilepsy

.jpg)
.jpg)




















