Polycythemia vera is a myeloproliferative disease that is associated with an overproduction of all blood cells and, as a result, an increased risk of thromboembolism. With an incidence of 1 to 2 diseases per 100,000 inhabitants annually, polycythemia vera is a rare syndrome disease.
What is polycythemia vera?

© fotomek - stock.adobe.com
As Polycythemia vera is a chronic myeloproliferative disease in which there is an increased synthesis of all blood cells, especially the erythrocytes, in the bone marrow.
As a result of this progressive and irreversible overproduction, an increase in hematocrit (cellular blood components) and blood viscosity (viscosity) is caused, which leads to microcirculatory disorders and an increased risk of thromboembolic events.
In addition, two clinical stages are differentiated in polycythemia vera. The first phase is characterized by increased erythrocyte synthesis and erythrocytosis (increased number of erythrocytes) and can be completely symptom-free. The progressive late phase is characterized by secondary marrow fibrosis (marrow tissue fibrosis) with extramedullary hematopoiesis (blood formation outside the bone marrow) and splenomegaly (enlargement of the spleen).
Polycythemia vera can also develop into myelodysplasia, in which blood formation is increasingly taken over by mutated stem cells, or acute myeloid leukemia.
causes
The exact etiology of the Polycythemia vera has not yet been clarified and is probably based on a mutative transformation of stem cells that have not yet been fully recorded, which can profile themselves into different specific cell types.
A so-called JAK2V617F point mutation was found in around 95 percent of those affected, which leads to an exchange of the amino acid valine with phenylalanine and thus to an increased division rate of the specifically affected cells. A functionally comparable JAK2 mutation in exon 12 (amino acid-coding DNA segment) was also observed in 2 to 3 percent.
Since these mutations also occur in other myeloproliferative syndromes such as essential thrombocythemia and primary myelofibrosis, possible triggering factors such as noxae (including benzene), ionizing radiation and the involvement of another, as yet unknown gene mutation are also discussed.
Symptoms, ailments & signs
Polycythemia vera is characterized by an excessive production of red blood cells (erythrocytes). As a result, the blood thickens and the flow properties deteriorate. The associated circulatory disorders can cause various complaints. Polycythemia vera often begins slowly, so that many patients initially show few symptoms.
Circulatory disorders in the hands and feet are among the more common symptoms. A lack of oxygen supply also causes the lips to turn blue (cyanosis). On the other hand, skin reddening appears on the face, arms and legs. Many patients with polycythemia vera complain of itching, especially after contact with water.
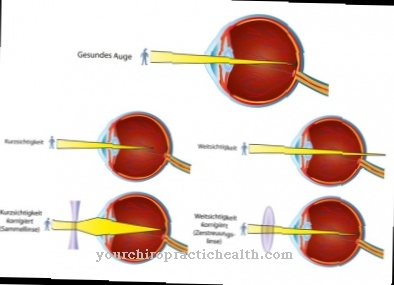
One speaks here of an aquagenic pruritus. The so-called erythromelalgia is also a characteristic symptom of the malignant blood disease. It is characterized by painful and sudden overheating and reddening of the feet and / or hands. The increased amount of erythrocytes can also lead to dizziness, nosebleeds, visual disturbances or ringing in the ears.
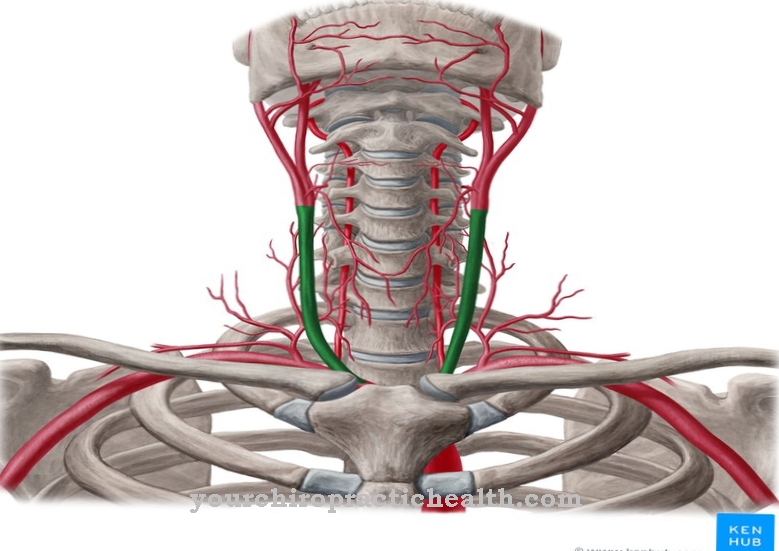
Due to the changed flow properties of the blood, there is also an increased risk of vascular blockages due to blood clots (thrombosis) or embolisms. A reduced blood supply to the coronary arteries, however, leads to a tightness in the chest (angina pectoris) and also increases the risk of a heart attack.
Diagnosis & course
A first suspicion of one Polycythemia vera in many cases results from an increased erythrocyte, hematocrit or hemoglobin value in the context of a blood test.
In addition, in many cases of the disease there is an increased leukocyte and platelet count with a simultaneous decreased erythropoietin level (EPO level). In the advanced stages of the disease, the suspicion can be corroborated by splenomegaly. The diagnosis is also confirmed by evidence of the JAK2 (V617F) point mutation.
In the differential diagnosis, polycythemia vera (primary erythrocytosis) must be differentiated from secondary erythrocytoses such as stress erythrocytosis, smoker erythrocytosis and erythrocytosis due to hypoxia or EPO-producing tumors in the liver or kidneys, which are characterized by an increased EPO level.
With early diagnosis and controlled therapy, the disease has a good prognosis with an almost normal life expectancy despite its chronic progression. If left untreated, polycythemia vera is associated with a significantly increased risk of thromboembolic events (including stroke, thrombosis, heart attack).
Complications
In this disease, patients primarily suffer from a significantly increased volume of blood. This also leads to reddening of the skin, which can be unpleasant, especially on the face, and thus significantly reduce the patient's quality of life. The blood itself is viscous, so that the coagulation is usually disturbed. The brain is also supplied with incorrect blood, which can lead to personality disorders or mood swings.
In many cases, people suffer from severe headaches or dizziness. Due to the illness, the risk of a stroke or a heart attack increases enormously, so that the life expectancy of the patient can be significantly reduced. In most cases, polycythemia vera is treated with medication.
Those affected are often dependent on long-term ingestion in order to minimize the risk of thrombosis. There are no particular complications or side effects. The life expectancy of the person affected may also be reduced due to polycythemia vera. A healthy lifestyle also has a very positive effect on the course of this disease.
When should you go to the doctor?
Disorders and irregularities in blood flow should be presented to a doctor. If there is a racing heart, dizziness, internal warmth or an unusual sensation of cold in some areas of the body, the person concerned needs help. A doctor should be consulted in the event of impaired perception, a tingling sensation in the limbs, numbness or hypersensitivity. Changes in the appearance of the skin, itching or redness should be presented to a doctor. If open wounds are found, sterile wound care is required.
If the person concerned cannot do this sufficiently, a doctor should be consulted. Otherwise germs can get into the organism and trigger further diseases or sepsis. This threatens a life-threatening condition.Bleeding from the nose or gums, a feeling of tightness in the organism and general functional disorders must be examined and treated. In the event of impaired vision or noises in the ears, the complaints should be clarified. If an acutely health-threatening situation arises, an ambulance service must be alerted.
An emergency doctor is required in the event of a disturbance of consciousness or a loss of consciousness. A sharp decrease in internal forces, a breakdown and sudden overheating are alarm signals for the body. Polycythemia vera can cause a blood clot to form. In severe cases, it comes to a stroke or a reduction in heart activity. Without emergency medical care, there is a risk of premature death.
Treatment & Therapy
A Polycythemia vera can so far only be treated causally or curatively by means of a stem cell transplant. Since such an intervention is associated with a high risk of secondary diseases and increased mortality, it is usually only considered in the very advanced stage of the disease.
On the other hand, palliative therapy measures aimed at reducing the risk of thromboembolic events, alleviating symptoms and preventing complications, are the focus of the treatment of polycythemia vera. To reduce the hematocrit value, bloodletting therapy (phlebotomy) is usually initiated, which ensures a quick and effective reduction in blood volume.
At the beginning, depending on the specific hematocrit value, a phlebotomy is carried out at two to three-day intervals, with the interval between the individual treatments increasing as the treatment progresses. To minimize the risk of thrombosis and to treat microcirculation disorders, a thrombosis aggregation inhibitor (low-dose ASA) is used at the same time.
If short intervals between the necessary phlebotomy sessions or high platelet counts can be identified, a drug-based reduction in the cell count using active ingredients such as hydroxurea or cytokines, which inhibit the synthesis of all blood cells in the bone marrow, is also sought as part of cytoreductive therapy.
In some cases in which a targeted reduction in the platelet count is indicated, anagrelide, which has a suppressive effect on platelet maturation, can be administered for the treatment of polycythemia vera.
prevention
There one Polycythemia vera can most likely be traced back to a mutation of stem cells whose trigger factors (triggering factors) could not yet be clearly clarified, the disease cannot be prevented. However, weight reduction, regular exercise, avoidance of long periods of sitting and consistent therapy for cardiovascular diseases minimize the increased risk of thromboembolism in polycythemia.
Aftercare
In most cases of polycythemia vera, patients have very few and only limited follow-up measures available. First and foremost, a quick and, above all, a very early diagnosis is important so that there are no other complications or further complaints. Therefore, those affected should consult a doctor at the first symptoms or signs of the disease in order to prevent further complications or complaints.
As a rule, self-healing cannot occur. The treatment itself takes the form of a minor surgical intervention. Afterwards, those affected should rest and take it easy. You should refrain from exertion and from physical or stressful activities in order not to unnecessarily burden the body. The medication should also be checked regularly and adjusted by a doctor.
If anything is unclear or if you have any questions about the medication, you should always contact a doctor first. Regular checks by a doctor are also very important in order to keep the blood count under permanent control. It cannot be universally predicted whether polycythemia vera will lead to a reduced life expectancy for those affected.
You can do that yourself
Self-help options are generally not available to those affected with polycythemia vera. In any case, the patient is dependent on treatment by a doctor, which involves a transplant of stem cells. In some cases, the patient dies despite treatment.
In general, the person affected with polycythemia vera must take care of their body and not expose themselves to unnecessary stress. Sports activities should also be avoided, as they strain the body. Stressful situations should also be avoided. In the event of itching, the affected area should not be scratched to avoid a rash. Due to the increased risk of a heart attack, regular examinations by a doctor are very useful in order to avoid a heart attack. Tests for tumors in the kidneys or in the liver are also useful, as these can also occur favored by polycythemia vera.
In some cases, contact with other people affected by the disease makes sense, as this leads to an exchange of information, which can be helpful for everyday life and make life easier. In most cases, polycythemia vera will reduce the patient's life expectancy.

.jpg)












.jpg)




.jpg)


