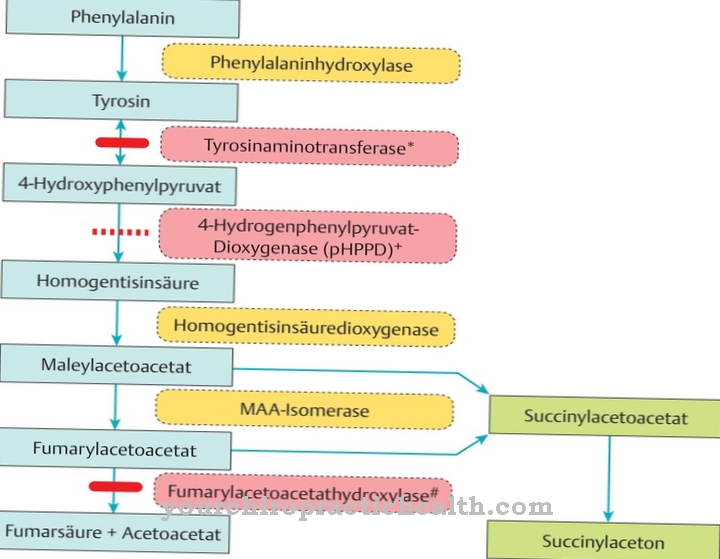
As arteriovenous fistula is an abnormal short-circuit connection that occurs between an artery and a vein. It is not uncommon for AV fistulas to appear in the head region.
What is an arteriovenous fistula?

© chanawit - stock.adobe.com
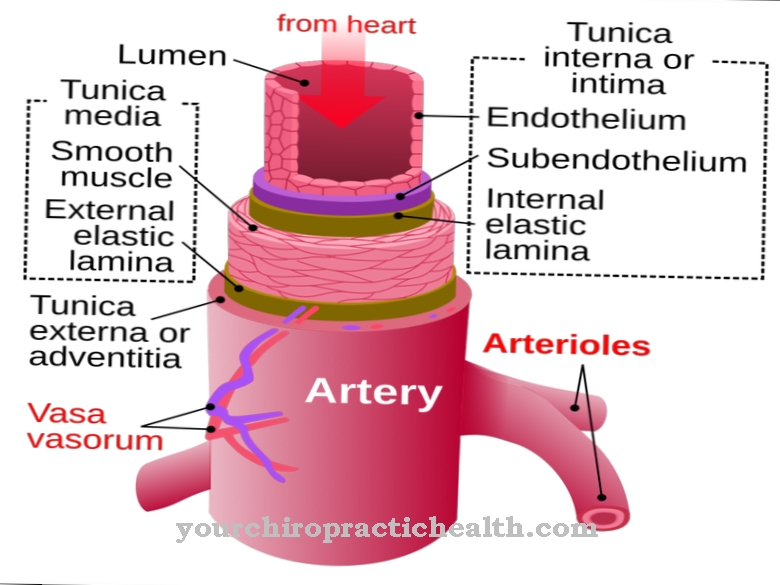
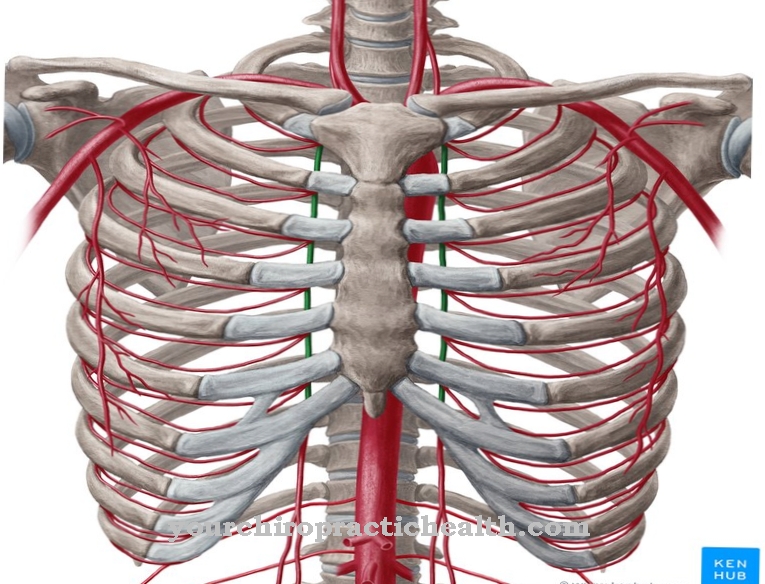
An arteriovenous fistula is an unnatural connection between the vein and the artery. It also bears the names AV fistula or Dural fistula. As a rule, the blood flow from the arteries takes place via the arterioles, the capillaries, the venules and finally the veins towards the heart. However, if there is an arteriovenous fistula, there is a direct flow of blood from the artery into the vein.
AV fistulas are either congenital or develop in the course of life. While congenital arteriovenous fistulas are very rare, acquired fistulas in most cases result from injury. This affects arteries and veins that are close together.
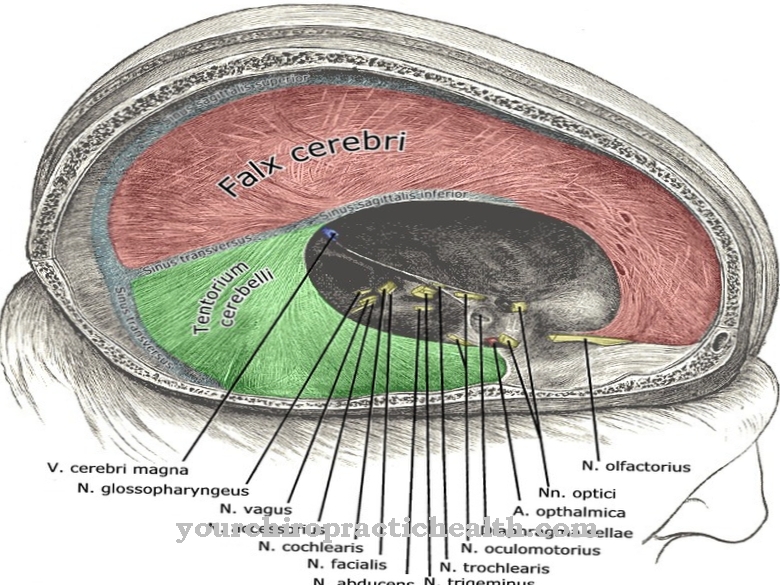
An arteriovenous fistula often occurs in the brain area. A dural fistula forms in the region of the dura mater (hard meninges). This unnatural connection leads to symptoms such as impaired vision or tinnitus. Arteriovenous fistulas are rare. Women over 40 are particularly affected by AV fistulas.
causes
The causes of the formation of an arteriovenous fistula are different. In addition to injuries to arteries and veins, thromboses (blood clots) in the sinuses, which are special blood vessels, can also be considered in the head area. In contrast to the actual veins, these vessels are stiff. They are also partly composed of the dura mater.
If a sinus vein thrombosis occurs, this results in the formation of abnormal blood vessels. This creates an unnatural connection between an artery and a vein. Injuries to veins and arteries are often caused by accidents, falls, or the action of violence that cause an acute opening between the artery and vein. In many cases, however, no specific cause for the development of an arteriovenous fistula can be determined.
The short circuit between the vein and the artery creates a risk of bleeding. While an artery is so stable that it can easily withstand higher blood pressure, the situation is different with the relatively thin-walled veins. The fistula between the artery and the vein increases pressure on the vein, which can cause blood to build up. If bulges form in the vein, the resistance of the vein wall also decreases, which in turn increases the risk of venous bleeding.
Symptoms, ailments & signs
If an arteriovenous fistula develops, different symptoms can occur. How these show up depends on the size and position of the AV fistula. A dural fistula in the head area is often associated with ringing in the ears (tinnitus). The affected person hears a pulse-like noise. It arises due to the increased blood flow to the blood vessels. Another common symptom of arteriovenous fistula formation is visual disturbance.
The reason for this is the build-up of blood, which results in increased pressure in the veins. This in turn has a negative impact on eyesight. In addition, the conjunctiva around the eye socket can become red and swell. If the increased pressure occurs on the cerebral veins, there is a risk of a dangerous stroke.
Another dreaded complication is the occurrence of life-threatening bleeding, which is rarely the case. How severe the symptoms are also depends on whether the fistula was caused by violence or indirectly. With traumatic fistulas, more intense symptoms are to be feared.
In some cases the vessels of the spinal canal are also affected by the AV fistula. Then, slowly, sensory disorders, weaknesses in the legs or difficulty urinating or defecating occur.
Diagnosis & course
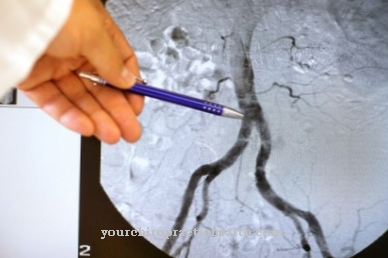
To diagnose an AV fistula, the treating doctor first looks at the patient's medical history. A physical examination will also take place, during which he will pay particular attention to neurological abnormalities. In order to specifically identify an arteriovenous fistula, imaging procedures such as angiography or magnetic resonance imaging (MRI) are carried out.
The course of the disease in an arteriovenous fistula depends on the start of therapy. If the treatment is not carried out on time, serious complications such as nervous failure or bleeding can occur. But the size of the AV fistula also plays an important role.
Complications
Complications that can be caused by an untreated atriovenous fistula (AV fistula) mainly depend on the diameter of the affected, directly connected, artery and vein and on their position. In principle, complications can be caused by profuse bleeding because the vein cannot withstand arterial blood pressure and tears occur. Complications caused by untreated AV fistulas in the body are usually manageable and reversible.
AV fistulas that have formed in the brain, on the other hand, can cause serious bleeding complications that can be accompanied by irreversible nerve damage and neurological failure. Basically, bleeding through AV fistulas in the brain poses a mortal danger because vital centers can be affected by the space occupied by the “leaked” blood. AV fistulas in the head are also called dural fistulas after the hard meninges dura.
With them, complications such as visual and hearing disorders arise even if the bleeding is not (yet) present. If there is bleeding in the brain - or in rare cases in the spinal cord - the affected nerves and ganglia are switched off, so that complications arise that are often comparable to those of a stroke. Complications that can show up with dural fistulas in the spinal cord include motor impairments in the legs, sensory deficits, and difficulties in keeping stool and urine under control (incontinence).
When should you go to the doctor?
An arteriovenous fistula does not necessarily need to be treated by a doctor. Medical advice is required if the fistula has not healed after three to five days at the latest or if accompanying symptoms occur. If there is accompanying itching, weeping or pain, a doctor must clarify the cause and, if necessary, initiate treatment immediately. If there is severe physical malaise or a fever, it is best to consult an emergency doctor.
The symptoms may be due to another illness that must be diagnosed in the hospital. If a reddish stripe is observed in the area around the arteriovenous fistula, there may be blood poisoning - an ambulance service must be alerted immediately. Risk patients with a fistula should always see a doctor.
The same applies to patients who have already suffered from a disease of the arteries. Otherwise, an arteriovenous fistula must be clarified if there is uncertainty about the symptom and the first symptoms occur. In general, the earlier a fistula is clearly diagnosed, the better the treatment options.
Doctors & therapists in your area
Treatment & Therapy
As part of the therapy of the arteriovenous fistula, attention is usually paid to avoiding bleeding. For this purpose, an endovascular embolization is carried out. In this method, the doctor uses a catheter to seal the abnormal blood vessel. The fine catheter can be inserted into the body through the arteries. The fistula is then treated with tissue glue or other materials.
There is also the option of closing the affected vessel from the vein side with special platinum coils. In some cases, a stent, an internal vascular splint made of wire, is also used. In this way the normal course of the vessel can be restored. Some patients also use a combination of several of these methods.
If these procedures fail to close the arteriovenous fistula, surgical intervention must take place. The surgeon cuts the AV fistula. However, there are certain risks involved in the surgical treatment of a dural fistula. This includes the undesired occlusion of a blood vessel.
Outlook & forecast
The arteriovenous fistula has a good chance of healing with early diagnosis and subsequent treatment. The fistula is more common in women over 40 years of age. Often there are already pre-existing conditions that worsen the prognosis.
Patients who refuse treatment or who take it too late must expect an acute condition. Bleeding can occur, which can lead to a stroke or heart attack. There is a threat of lifelong impairment or premature sudden death.
If treatment is provided in good time, there are good prognostic prospects for patients without any other previous illnesses. There is a surgical procedure that is completely completed within a few hours. The patient then needs some healing time and can be discharged as symptom-free after a few weeks or months.
Everyday life must be adapted to the new circumstances and check-ups should be performed. Nevertheless, the patient can go about his everyday life himself under normal conditions. If no further sequelae have occurred, there will be no further treatment measures after the procedure.
Alternatively, individual therapeutic approaches are offered to treat the consequences of the arteriovenous fistula. Functional disorders such as impaired hearing or vision are treated with appropriate equipment. In the case of nerve damage, there is an increased risk that it can no longer be successfully corrected.
prevention
Effective preventive measures against the development of an arteriovenous fistula are not known.
Aftercare
In most cases, the person affected does not have any special measures and options for follow-up care available, so that first and foremost an early examination and treatment by a doctor must take place. There is also no independent healing, so treatment by a doctor must take place in any case.
The earlier the disease is recognized by a doctor, the better the further course of the disease will usually be. In most cases, the life expectancy of the person affected is not reduced or otherwise restricted. The treatment itself takes the form of a small surgical procedure, which usually runs without complications.
After such an operation, the person concerned should definitely rest and continue to protect his body. Exertion or other stressful physical activity should be avoided. Above all, the affected area on the body should be spared and protected.
Regular examinations by a doctor are also necessary after the procedure. Further follow-up measures are no longer necessary. In many cases, other diseases can also indicate this fistula, so that a doctor should be consulted at the first signs and symptoms.
You can do that yourself
An arteriovenous fistula (AV fistula) is a vascular connection between an artery and a vein. This leads to a short circuit between the arterial and venous side of the blood circulation, bypassing the capillary system. The connections are usually formed by an injury with bleeding, which in rare cases can stimulate the formation of the fistula.
The symptoms that occur depend on the size of the fistulas and the arterial and venous vessels involved, as well as their location. If the fistulas are smaller outside the brain and there are hardly any symptoms, self-help measures or an adjustment in everyday life are not necessary. In many cases, however, the unwanted fistulas form in the brain in the area of the hard meninges (dura mater). The hearing and visual centers are often affected. For example, tinnitus and visual disturbances can set in.
Because of the uncertain prognosis about the further course of the disease, in these cases it is not so much an adjustment in everyday life or the use of self-help measures that is required, but rather an exact diagnosis and possible treatment that should prevent the progression of the disease and the associated serious symptoms. In the head area, there is a particular risk of bleeding, which takes up space and can cause mild to serious neurological deficits.


.jpg)

.jpg)





.jpg)
.jpg)
.jpg)







.jpg)