As Preimplantation Diagnostics Doctors refer to molecular genetic studies. Hereditary diseases or anomalies in the chromosomes of embryos that arise during artificial insemination are researched.
What is Preimplantation Diagnostic?

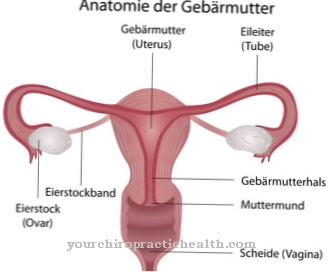
In pre-implantation diagnostics (PID) are medical examinations of embryos that are created by artificial insemination. The embryos are only a few days old and are examined before they are transplanted into the female uterus. In this way, it is the doctors u. a. possible to detect defects in chromosomes that pose a risk of miscarriage or stillbirth.
The parents can then decide whether the transplant will take place in the uterus or not. Preimplantation diagnosis is one of the controversial medical procedures. Although the method has been used since the 1990s, it has only been approved in Germany since 2011.
Function, effect & goals
Pre-implantation diagnostics are used to reveal genetic changes that indicate serious illnesses in the unborn child. The genetic material of artificially fertilized egg cells is checked for chromosomal disorders and hereditary diseases. The prenatal diagnostic method is only carried out in risk groups who are suspected of having a genetic disease.
This can be the case, for example, if Huntington's disease has occurred several times in a family. There is also the possibility that the woman has already had several failed artificial inseminations (in vitro fertilization).
However, the results of pre-implantation diagnostics are not always absolutely certain. In rare cases, misdiagnosis is quite possible. An additional prenatal diagnosis (PND) such as a chorionic villus sampling or an amniotic fluid test can be carried out to confirm the diagnosis. The genetic diseases for which pre-implantation diagnosis makes sense are primarily Huntington's disease, sickle cell anemia, cystic fibrosis, beta thalassemia and Marfan's syndrome.
Further diseases are the Patau syndrome (trisomy 13), the Edwards syndrome (trisomy 18), monosomy 21 and the muscular dystrophy of the Duchenne type. In the meantime, PGD is not limited to detecting around 200 hereditary diseases. It also serves to increase the success rate of artificial insemination and to select the sexes, although it does not necessarily have to be related to a disease. In addition, pre-implantation diagnostics also identify diseases that can be examined as part of prenatal diagnostics, but for which, as a rule, no diagnosis is made.
The most common area of application of PGD is aneuploidy screening. This is increasingly used in infertile couples who are already of an advanced age and who have already had several unsuccessful attempts at in vitro fertilization or miscarriages. As part of the pre-implantation diagnosis, the embryos that are responsible for the problems that arise should be separated out. In this way, the chances of success in having a healthy child can be increased.
In some countries, PGD is also used to identify so-called rescuer siblings. This refers to embryos that can help older siblings who are suffering from a serious illness by donating umbilical cord blood or bone marrow. For this purpose, pre-implantation diagnostics selects the appropriate tissue characteristics following artificial insemination.
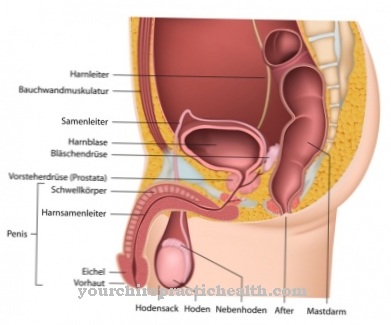
In order for a pre-implantation diagnosis to take place, artificial insemination must first take place. This leads to the formation of several embryos. The fertilization of the female egg cells with the male's sperm takes place outside the body. After the egg cells have been aspirated from the woman's body, they are developed into embryos in a test tube. Around three days after fertilization, one or two cells can be removed and examined as part of the pre-implantation diagnosis, for which different techniques are used.
You can find your medication here
➔ Medicines for painRisks, side effects & dangers
Pre-implantation diagnostics are always associated with the risks associated with artificial insemination. This major procedure can lead to side effects such as pain, breathing difficulties, nausea and blood clotting disorders.
In addition, a complication must be expected, which is more common with artificial insemination in connection with PGD than with other procedures. This is ovarian hyperstimulation syndrome (OHSS). It is divided into easy and severe course forms. The severe forms can even be fatal.
Basically, the woman receives numerous hormones during artificial insemination in order to allow the egg cells to mature in the ovaries. In pre-implantation diagnostics, the amount of hormones must be even higher than in a simple test tube fertilization without PID. However, this creates the risk of overstimulation of the ovaries, which is noticeable by their strong enlargement. Cysts form inside the ovaries and the size of the abdomen increases. In some affected women, fluid can also collect in the abdominal region. In addition, the blood increases in thickness, which in turn causes circulatory disorders in the kidneys. As a result, there is a risk of dangerous kidney failure.
Preimplantation diagnostics is a procedure that has been highly controversial around the world for years. During the discussions, fundamental ethical and political questions about the value of life are raised. Critics accuse PGD of not accepting social diversity. In addition, the pressure on parents to have healthy children is increasing. The approval of pre-implantation diagnostics in Germany would damage the value system of the Basic Law on the right to dignity. However, the proponents of PGD see the process as an opportunity to spare couples and their children from serious hereditary diseases.



.jpg)









.jpg)
.jpg)


.jpg)