A progressive systemic scleroderma (PSS) is a chronic inflammatory disease of the connective tissue and the vascular system, which is caused by a dysregulation of the body's own immune system. Progressive systemic scleroderma is more common in women than men.
What is Progressive Systemic Scleroderma?

© Henrik Dolle - stock.adobe.com
As progressive systemic scleroderma (PPS) is a chronic inflammation of the connective tissue and the vascular system of the skin and internal organs, which can be traced back to a disturbed immune system (autoimmune disease).
In the case of progressive systemic scleroderma, a dysregulation of the immune system attacks the body's own collagenous connective tissue (collagenosis) and causes inflammatory reactions that lead to a loss of elasticity of the skin and, later, of the organs and hardening (sclerosis).
This leads to edema in the fingers and hands as well as sclerodactyly, the mask face characteristic of progressive systemic scleroderma due to loss of expression, swallowing disorders due to the shortening of the ligaments of the tongue and inflamed joints (arthralgia).
causes
The one for one progressive systemic scleroderma Typical symptoms are caused by a disruption of the immune system, whereby the immune system attacks the body's own structures, especially the collagenous connective tissue and vascular system of the skin and internal organs, and causes inflammatory reactions.
In addition, with progressive systemic scleroderma there is a dysregulation of certain cells of the connective tissue (fibroblasts), as a result of which they increasingly synthesize collagen, which is deposited in the skin and the skin and, in the further course, the connective tissue and connective tissue characteristic of progressive systemic scleroderma Causes vascular changes in the internal organs.
The triggers for this dysregulation are not yet known. In addition to genetic factors, viral and bacterial antigens as well as certain drugs, tumors, UV light and sex hormones are discussed as triggers for progressive systemic scleroderma.
Symptoms, ailments & signs
The symptoms of progressive systemic scleroderma can be divided into three stages. First of all, changes and thickening of the skin on the hands and feet are noticeable. The initial stage of progressive systemic scleroderma is also characterized by edema on the hands.
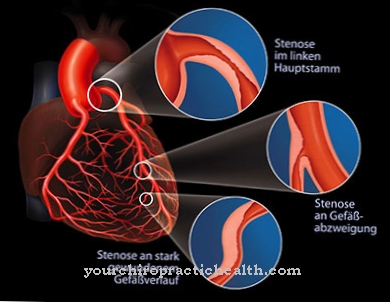
The connective tissue hardens increasingly. It breaks down. Raynaud's syndrome is also typical. This is characterized by whitish-bluish hands with poor blood circulation. Sometimes at this stage there is necrosis of the stretched skin areas that are stressed by hardened scar tissue.
The facial expressions are increasingly reduced. The progressive skin tension creates mask-like facial features. Since the lip region can also be affected by increasing tissue hardening, radial folds often form around the mouth opening. The mouth becomes increasingly smaller. Medically one speaks of a microstomy.
Small blood vessels on the face often expand into telangiectasias. The skin pigmentation can also be noticeably changed. In the second stage, the inflamed and edema-burdened joints can no longer be moved freely and painlessly due to the increasing tightening of the skin. Progressive systemic scleroderma causes the fingers or toes to curve.
The third stage of progressive systemic scleroderma affects internal organs. These too are increasingly affected by hardening. This leads to hardened digestive organs, pulmonary fibrosis and difficulty swallowing due to sclerotic changes in the esophagus and mouth.
Diagnosis & course
A progressive systemic scleroderma is diagnosed on the basis of the symptoms present, especially the skin changes. The diagnosis is confirmed by a tissue removal and analysis (biopsy) from the affected skin areas as well as a blood test.
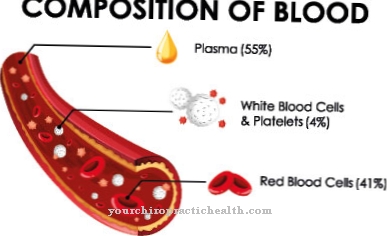
In the presence of progressive systemic scleroderma, the concentration of certain immunological proteins, the so-called antinuclear antigens, and the ESR (blood sedimentation rate) are increased.
Furthermore, the stage-dependent vascular changes characteristic of progressive systemic scleroderma can be determined by a capillary microscopy of the nail bed. A possible dysphagia can be diagnosed by measuring the pressure in the esophagus (esophagus). In addition, cardiac sonography (ultrasound) and an analysis of the lung function provide information about organ involvement.
Progressive systemic scleroderma can have two different forms. The so-called acral scleroderma has a locally limited course in which only smaller areas of the skin, especially on the feet and hands (acres), are affected. The prognosis is usually good if there is no lung involvement.
In the diffuse form of progressive systemic scleroderma, the internal organs (kidneys, lungs, heart) are usually involved, which means that the prognosis and course are poor (unfavorable) depending on the extent of the involvement.
Complications
Most of the complications in a diagnosis such as progressive systemic scleroderma are to be feared because of internal organ involvement. In this form of scleroderma, it is not only the skin that is affected by hardening. The immune system is also involved in this rare autoimmune disease due to overreactions. It is all the more important that those affected receive long-term treatment in order to avoid complications.
Nicotine consumption can make the symptoms of progressive systemic scleroderma even worse. In smokers, the vessels, which are already constricted, become even more narrow. The increased tendency to inflammation is increased. In this severe form of scleroderma, the narrowing of the vessels must also be reduced with measures against the effects of cold. With inadequate nutrition, hydration and skin care, the affected person's skin dries out. The disease can lead to swallowing disorders, circulatory disorders of the fingers or a mask face.
Inflammatory flare-ups, intestinal problems and immunodeficiency are common in those affected. Complications in scleroderma can also occur in the musculoskeletal system. Without lymphatic drainage or physiotherapy, the joints stiffen increasingly. Moderate sports such as swimming are also advisable.
In the third stage of the disease, pulmonary fibrosis can occur. Other organs can also become inoperable due to increasing tissue hardening. Since the life expectancy is reduced with progressive systemic scleroderma, the treatment is correspondingly intensive.
When should you go to the doctor?
Changes in the appearance of the skin, swelling, discoloration or growths should be presented to a doctor. If edema, thickening of the skin layers or peculiarities of the limbs develop, a check-up visit with a doctor is advisable.
Increasing complaints or persistent irregularities should be examined and treated. If there are abnormal expressions, there is cause for concern. If you notice mask-like facial features or a restricted facial expression, a doctor's visit is required. Hardened lips in the area of the lips are characteristic of progressive systemic scleroderma. The complaints must be clarified so that a treatment plan can be drawn up. In addition, the shape of the mouth, and in particular the opening of the mouth, becomes smaller and smaller in the course of time.
If visible blood vessels develop on the face, restrictions in the act of swallowing or visual changes in the oral cavity, a doctor should be consulted. Any abnormalities in the esophagus and a decrease in food intake should also be examined. General malfunctions, induration inside the body or a feeling of tightness should be presented to a doctor.
The disease leads to changes in the organs that must be treated so that there are no complications or life-threatening conditions. Circulatory disorders, a feeling of illness or general malaise should be clarified by a doctor. A doctor should be consulted if performance drops or if immune system disorders are noticed.
Treatment & Therapy
The therapeutic measures are aimed at one progressive systemic scleroderma on a reduction and elimination of the symptomatic complaints and a slowing down of the progressive course.
In particular, anti-inflammatory drugs such as NSAIDs (non-steroidal anti-inflammatory drugs such as diclofenac) and glucocorticoids are used for inflammatory flare-ups. Immunosuppressants (methotrexate, cyclophosphamide) are also used to minimize and inhibit the dysregulation of the immune system that is present in progressive systemic scleroderma.
In addition, physiotherapy, occupational therapy, heat therapy and physical measures to maintain joint mobility as well as careful skin care with moisturizing ointments and lymphatic drainage are recommended. In the presence of circulatory disorders, vasodilating substances (prostaglandins) and acetylsalicylic acid can also be used, while in progressive systemic scleroderma with kidney involvement, antihypertensive agents (ACE inhibitors) can also be used as medication.
In some cases of progressive systemic scleroderma, surgery may be required to remove skin defects or stiff joints. Active ingredients such as interferon, which inhibits the formation of new connective tissue, and tacrolimus, which suppresses an enzyme involved in the immune system (calcineurin), are in a trial phase. Positive experiences were also made with infused iloprost in progressive systemic scleroderma.
You can find your medication here
➔ Medicines against edema and water retentionprevention
As the trigger for the dysregulation of the immune system progressive systemic scleroderma are not known, the disease cannot be prevented. However, a few simple measures can alleviate the symptoms. Saliva-stimulating candies (peppermints, chewing gum) and more frequent but smaller meals can alleviate swallowing problems and prevent dry mouth. In order to avoid the cold, it is recommended that people with progressive systemic scleroderma move their annual vacation to the winter months and to warm regions.
Aftercare
Progressive systemic scleroderma is a subgroup of scleroderma, which is an incurable autoimmune disease. Therefore, direct follow-up care is not possible in this form and a rather permanent treatment of the mostly chronically worsening disease is necessary. After a diagnosis and acute treatment, long-term treatment must follow as well as reducing, delaying or preventing possible late effects in the course.
In severe forms of the disease, these consequences can ultimately lead to the death of the patient. As a rule, the person affected is dependent on a variety of medications for life and regular visits to specialist doctors are essential. The concrete course and a direct prognosis are not foreseeable, there are very different forms here.
Finally, when it comes to aftercare, palliative care should also be mentioned if it becomes clear that the disease will inevitably lead to death within a certain time. The patient's quality of life can be increased or maintained at a very good level for as long as possible. One should not be afraid to contact trained doctors and nurses in palliative care in good time and to take into account the wishes of the person concerned.
You can do that yourself
It is particularly important for those affected to receive permanent medical care. Independently discontinuing or changing the medication of prescribed drugs can lead to complications or an increase in the existing symptoms.
Since the consumption of nicotine leads to a deterioration in health and an intensification of the existing discrepancies, this should be completely avoided. Likewise, environments in which people smoke should be avoided. The patient's organism reacts even if the nicotine is only absorbed passively.
Although the disease is triggered by a disorder of the immune system, the body's defenses should still be sufficiently strengthened. A healthy lifestyle and a balanced diet contribute to strengthening your well-being. Obesity should be avoided and sufficient exercise should take place.
Progressive systemic scleroderma is accompanied by visual changes. To avoid mental or emotional problems, it is necessary to strengthen self-esteem. Otherwise, mental illness may develop. As a balance, care should be taken to ensure a stable social environment and leisure activities should be aimed at strengthening the joy of life.
Yoga or meditation techniques can be helpful in relieving stressors. These can be carried out independently by the person concerned at any time.



.jpg)





















