At Pseudomonas it is gram-negative, aerobic, actively moving and rod-shaped bacteria. They move with polar flagella and do not form spores. They can cause various diseases in humans.
What are Pseudomonas
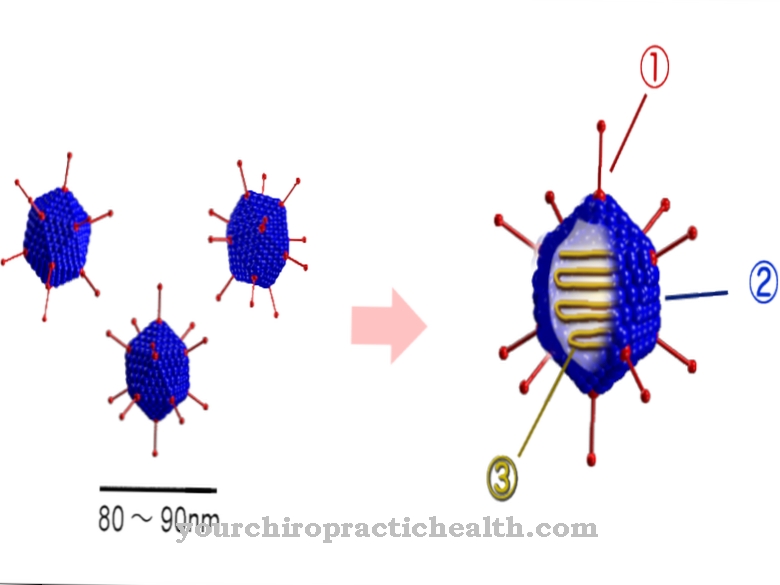
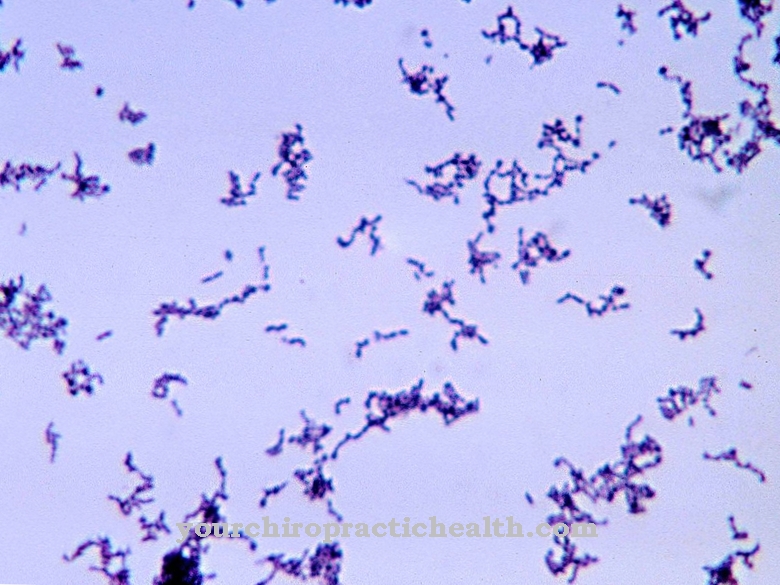
Pseudomonas are a genus of bacteria that are gram negative. So they only have a single-layer, thin murein envelope (cell wall). This gives the bacterium strength. The bacteria are in the form of rods, actively move with polar flagella, are aerobic and do not form spores. Pseudomonas are classified in the group of nonfermenters, so they are not capable of fermenting glucose. Rather, they utilize them oxidatively.
Pseudomonas are considered to be physiologically highly flexible. These bacteria are so-called opportunists, i.e. facultative pathogens. Thus, when the host immune system is weakened, Pseudomonas cause disease.
Occurrence, Distribution & Properties
Pseudomonas are ubiquitous. So they occur everywhere in the environment. These bacteria are often referred to as “puddle germs” because they live in the ground, in water, on plants and animals. Pseudomonas therefore prefer primarily moist habitats. The bacteria do not belong to the normal flora of humans. If they are detected in water installations, this indicates the presence of hygienic problems.
Pseudomonas reach a size between 0.5 to 1.0 x 1.5 to 5.0 µm. Since the bacteria are aerobic, they usually need oxygen for their energy metabolism. The majority of Pseudomonas are resistant to antibiotics. With a higher cell density, they also have the ability to form biofilms. With this they are protected from antibiotics and phagocytes.
Of this group, Pseudomonas aeruginosa is the most common pathogenic agent in humans. The name is derived from the Latin "aerugo" for verdigris and indicates the color of purulent wound secretion. The germ was discovered in 1900. Pseudomonas auruginosa is mainly found in humid environments and is a widespread soil and water germ. It is about two to three micrometers in size and has tufted lophotric flagella. A fixation on surfaces is possible by means of adhesive frames.
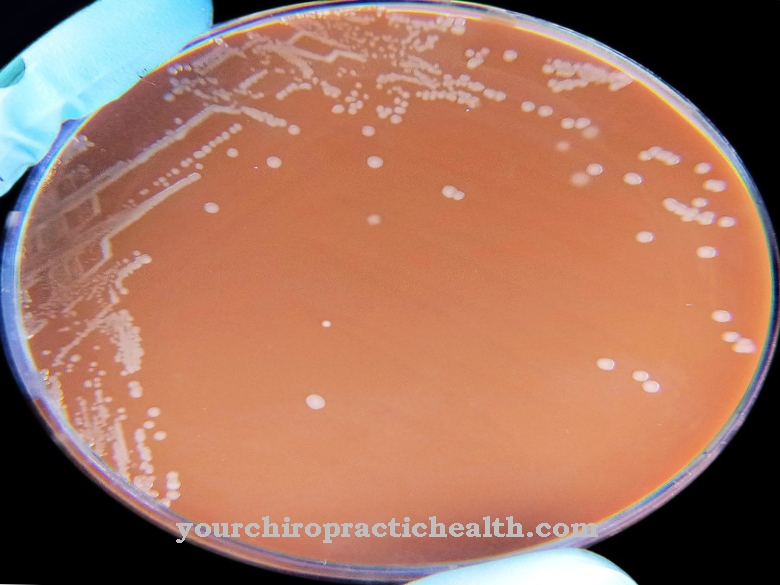
As a gram-negative bacterium, Pseudomonas aeruginosa turns red in the Gram stain (diagnostic agent in medical and scientific microbiology). The pathogen is very undemanding in terms of its living conditions and can - even if it prefers a moist habitat - survive for a long time in dry areas.
Pseudomonas aeruginosa is a so-called nosocomial germ. Infections with it occur primarily in hospitals (e.g. in drugs, in dialysis machines, in urine bottles, in disinfectants), which is why we also speak of hospital germs. Transmission from hospital staff to patients is also possible; infections only occur in direct contact with the pathogen.
Some Pseudomonas species produce TTX (tetrodotoxin), a highly dangerous neurotoxin. The high pathogenicity - especially in Pseudomonas aeruginosa - is attributed to various virulence genes.
Illnesses & ailments
In people with an intact immune system, Pseudomonas usually cannot cause diseases. However, if the immune system is weakened (e.g. after operations or in patients with HIV infection), the risk of a Pseudomonas infection is significantly higher. Infections with Pseudomonas can become noticeable in many areas of the body (e.g. skin, bones, ears, eyes, urinary tract, heart valves, subcutaneous tissue). The localization of such an infection depends on the entry point of the pathogen. The first sign, especially in hospital patients, is so-called gram-negative sepsis (blood poisoning).
Pseudomonas often colonize burn wounds. Sometimes so massive that it leads to bacteremia. Pseudomonas aeruginosa in particular penetrates deep cuts. Purulent wound secretion then has a typical blue-green color and a sweet to fruity odor.
Furthermore, Pseudomonas cause otitis externa (inflammation of the outer ear), which occurs mainly in tropical regions, in which purulent secretion escapes from the ear. Malignant otitis externa mostly occurs in patients with diabetes. It is much more severe and characterized by severe earache and often unilateral cranial nerve paralysis.
The so-called ecthyma gangrenosum is a pathognomonic skin lesion in neutropenic patients and is characterized by centrally ulcerated, erythematous and purple-black areas with a diameter of about one centimeter. They often occur in the armpit as well as in the anogenital area (area around the anus and genitals). In addition, skin and soft tissue infections can lead to inflamed paranasal sinuses, cellulitis (pathological changes in connective tissue) or osteomyelitis (infectious bone marrow inflammation).
Pseudomonas aeruginosa can cause ventilation-associated pneumonia. Pneumonia or sinusitis are more common in patients with HIV infections. If cystic fibrosis is present, Pseudomonas bronchitis can develop later. In addition, Pseudomonas very often lead to infections of the urinary tract, especially after urological operations.
The eyes can also become infected, often after trauma or from contamination of contact lenses or the cleaning fluid. In rare cases, Pseudomonas can cause acute bacterial endocarditis. As a rule, it affects artificial heart valves after open heart surgery or native valves in drug abuse.
In many cases, a Pseudomonas infection also leads to bacteremia. If patients are not intubated, there is no evidence of urological complaints and if other species than Pseudomonas aeruginosa are also involved in the infection, it was probably caused by contaminated infusion solutions, disinfectants or medication.
The pathogen is detected by creating a culture from the secretion of the infection site. Blood or urine can also be used for this. Third-generation cephalosporins (e.g. cefepime), acylaminopenicillins (e.g. piperacillin), carbapenems, fluoroquinolones and aminoglycosides are used to treat infections with Pseudomonas.