Papillomaviridae are viruses that cause skin changes in humans and animals. Depending on the host organism, the viruses are very specific. The largest percentage of this group of viruses is made up of the human papilloma viruses (HP viruses or HPV), which only affect humans. The viruses are transmitted through skin contact and are widespread.
What are Papillomaviridae?
The Papillomaviridae (lat. Papilla = wart) form their own virus family with the genus of the wart viruses. Papilloma viruses cause tumors of the skin and mucous membranes in humans and animals, which are usually benign.
So far, around 150 different virus types are known, which are divided into three classes according to the affected body region (genital area, oral mucous membrane or skin). Depending on the type and individual genetic factors as well as environmental influences, there is a risk of degeneration and development of cancer.
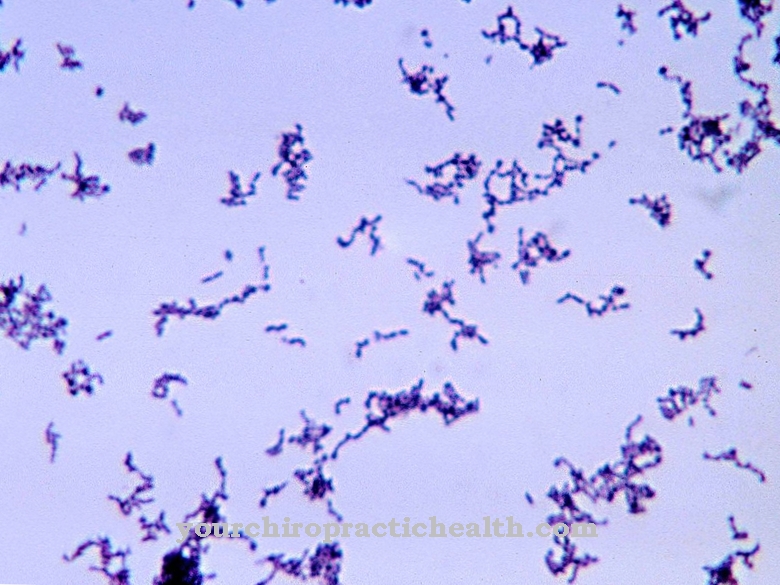
The infection occurs through skin contact, as the papilloma viruses penetrate the skin and mucous membrane through the smallest injuries and multiply there.
Occurrence, Distribution & Properties
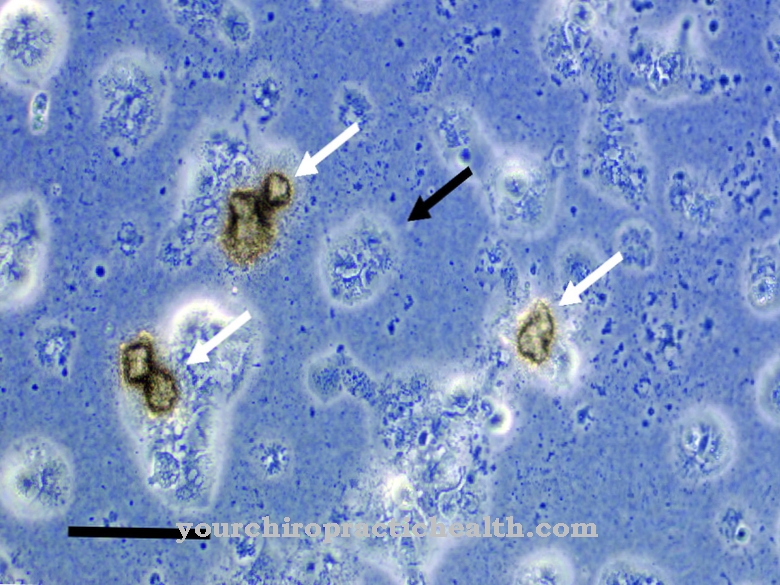
The genetic material of the virus is found in double-stranded, circular DNA. Papilloma viruses do not have a virus envelope, which means that they leave infected cells by destroying the host cell. Papillomaviridae are widespread due to their easy transferability and, for example, form skin warts on hands or feet or infect skin and mucous membrane cells in the genital area.
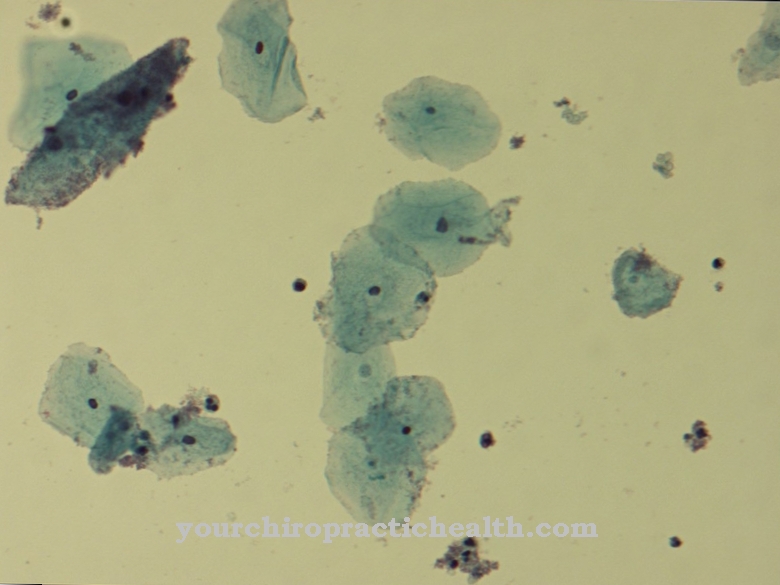
The genital types make up the largest share and can cause various diseases such as genital warts. Often these warts are not visible or they develop into solid nodules. They usually occur more frequently and often have a whitish, sometimes reddish appearance and can cause symptoms such as itching or burning.
The genital viruses are divided into low-risk and high-risk types depending on the assumed probability of cancer. Low-risk viruses have almost never been found in cancer and cause harmless genital warts, viral warts of the mucous membrane, the oral mucosa or juvenile flat warts. As potentially life-threatening pathogens, the “high-risk” viruses have been shown to be involved in the development of cervical cancer. They have also been detected in other cancers of the genital organs and the mouth and throat.
The infection runs through skin contact, with genital virus types through unprotected sexual intercourse. HP virus infection is one of the most common infectious venereal diseases. The infection is also favored by the fact that the infection of a part of the body with HP viruses is often not visible and the viruses can remain inactive for years. An infection usually goes unnoticed and in most cases disappears by itself without the person affected having any symptoms. Scientific studies assume that most sexually active women and men become infected with HPV at least once in their lifetime. Acute infections can easily be detected by an HPV test of a mucous membrane swab or a tissue sample. Since papilloma viruses can mutate into cancer precursors, this test has been carried out for many years as a standard by gynecologists as part of the early detection of cervical cancer.
In Germany there has been a vaccine against certain types of the human papillomavirus since 2007. The Standing Vaccination Commission (STIKO) has since recommended vaccinating girls between the ages of 12 and 17. Depending on the age, two to three doses of vaccine are necessary and the statutory health insurance companies usually bear the costs for the measure. In the meantime, further developed vaccines are being tested that destroy cells and tumor cells that are already infected with HPV.
Since not all skin contact is avoided during protected sex, condoms do not offer adequate protection against this sexually transmitted disease. In addition to completely renouncing sexual contact, vaccination is the safest protection against the infectious viruses.
Illnesses & ailments
Depending on the type, infections caused by the papillomavirus usually heal on their own. Possible therapies for treating warts range from local treatment with creams or solutions to the surgical removal of bothersome or pronounced warts and cell changes. In the worst case, however, a persistent infection with HP viruses can develop into cancer without treatment, as the cell changes only occur through the permanent settlement of the virus. The most well-known type of tumor is cervical cancer (cervical cancer). As a therapy, oncologists then weigh up between surgery, chemotherapy or radiation therapy, although one of the methods is sufficient for many sufferers. Sometimes a combination of radiation and chemotherapy is necessary. Concomitant medication to prevent infections supports the therapy.
Tumors can also develop in the genital area and in the mouth and throat, as well as so-called head and neck tumors. Smoking, an existing herpes infection, long-term use of contraceptive medication or a weakened immune system are considered to be cancer-promoting factors.
A less dramatic, but quite serious effect is the mutual contagion in permanent partnerships. With the so-called ping-pong effect, it cannot be clarified who infected whom first. Basically, both partners seem to infect each other again and again. Doctors therefore always assume that both partners are infected and adjust the treatment accordingly. It is therefore generally advisable to consult a dermatologist or family doctor if there are abnormalities on the skin or in the genital area, especially if there are additional complaints.





















.jpg)



