Pseudomycoses show the clinical picture of mycoses. Unlike a mycosis, one lies Pseudomycosis not a fungal infection, but a bacterial infection. The therapy depends on the pathogen and the pattern of the infestation, but usually encompasses the administration of antibiotics.
What is pseudomycosis?

© SpicyTruffel - stock.adobe.com
Mycoses are associated with microorganisms. They are fungal diseases that correspond to an infectious disease. The causative agents of the infection are mycelial fungi and yeasts. The process of infection does not necessarily have to lead to illness. The pathogens of a mycosis spread parasitically in living tissue.
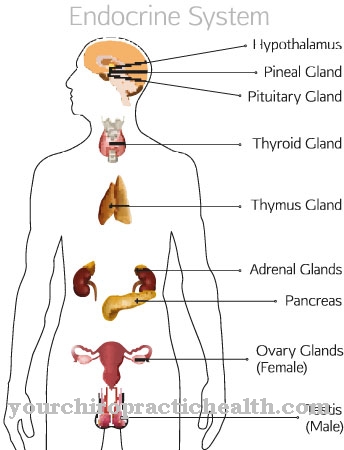
The clinical picture of mycoses is relatively typical. The infestation usually manifests itself in red, oval or round lesions of the skin or mucous membranes, which are marginally scaly and subjectively associated with itching or burning. A Pseudomycosis shows the clinical picture of mycosis, but is not caused by fungi. The colonization can affect the skin, the lungs, or the central nervous system.
In most cases, pseudomycoses are reactions to various types of bacterial pathogens. In addition to nocardia, actinomycetes and bacteria of the species Corynebacterium minutissimum can lead to a mycosis-like clinical picture. In the case of actinomycetes in particular, the infection often corresponds to an endogenous infection.
The bacteria of the normal skin or oral flora penetrate deeper tissue layers. In extreme cases, pseudomycoses can cause bacteremia and the associated sepsis. Depending on the pathogen, the symptoms and the predominantly affected tissue differ.
causes
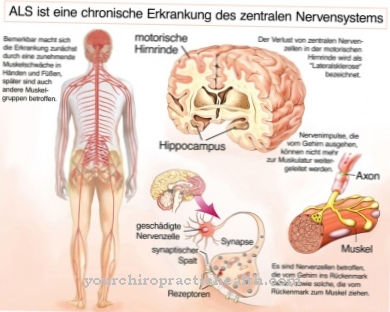
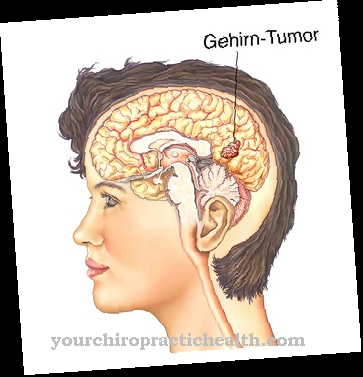
Depending on its cause, pseudomycosis is divided into different subgroups. Infections with nocardia and in particular the bacterium Nocardia asteroides cause so-called nocardiosis, which manifests as pseudomycosis in the central nervous system and in the lungs.
Another causative agent of pseudomycoses are bacterial actinomycetes, which can cause what is known as actinomycosis or radiation fungal disease and manifest themselves in the form of pseudomycosis in various parts of the body. Actinomycoses are divided into cervico-facial, thoracic and intestinal forms depending on the tissue affected and thus the course.
Actinomycetes in particular resemble the shape of mushrooms in their morphology and are therefore often referred to as ray fungus. The most common causative agent of this pseudomycosis is the species Actinomyces israelii, which naturally inhabits the human mouth as a commensal. Infections with the Corynebacterium minutissimum, which lives in the normal skin flora and mainly causes mycosis-like skin symptoms.
With this cause, the pseudomycosis is also called Erythrasma designated. What all pseudomycoses have in common is their bacterial origin, which is the primary criterion for differentiating them from real mycoses. As a rule, immunosuppressed or otherwise immunodeficient patients are at risk for pseudomycoses.
Symptoms, ailments & signs
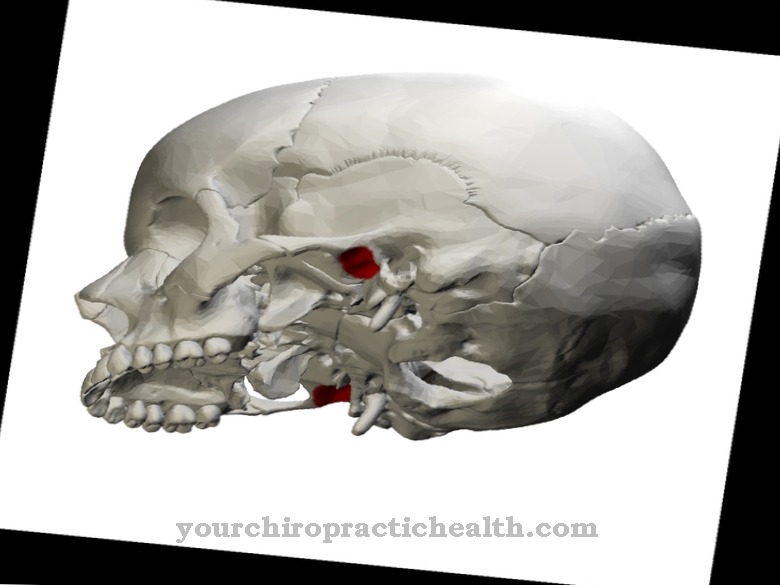
Patients with nocardiosis show the symptoms of a granulomatous infectious disease and are often affected by pneumonia, brain abscesses, endocarditis, or empyema. Actinomycoses are also associated with abscess formation. The accumulations of pus from bacteria and dead cells spread to the surrounding tissue, with the tough, consistent lesions framed by connective tissue and granulation tissue.
In addition to the skin, these pseudomycoses can affect the lungs, the chest area, the abdominal organs and mucous membranes, the central nervous system or the face, neck and mouth area. Erythrasma typically manifests itself in turn in the form of skin symptoms that appear as sharply defined, brownish-red, flat areas of skin with fine wrinkles and scales. This pseudomycosis can be accompanied by itching.
This variant occurs most often in the armpits, in the groin region, on the scrotum or in the spaces between the toes, with the infection spreading to other regions of the skin. All bacterial infections can be accompanied by general signs of infection such as fatigue, tiredness, fever, and chills.
If the central nervous system is involved, functional impairment of sensitivity or motor skills may occur. When the bacteria reach the bloodstream, blood poisoning can develop in patients with poor immune systems.
Diagnosis & course of disease
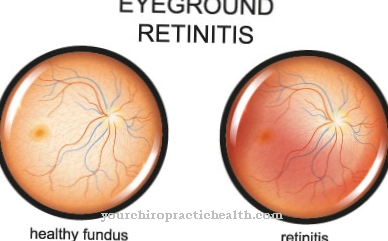
The diagnosis of pseudomycosis is usually based on cultural evidence of the typical pathogen. However, this detection takes some time, especially with actinomyces, so that the microscopic view often has to serve as a diagnostic criterion. The involvement of organs and mucous membranes is assessed more closely using imaging techniques.
The prognosis of the patient differs depending on the type of pathogen and the pattern of infestation. Sepsis can be a life-threatening situation. Untreated nocardiosis are usually fatal. Erythrasms are associated with the best chance of recovery.
Complications
In severe cases, pseudomycoses can cause bacteremia and, as a result, sepsis. In bacteremia, bacteria invade the bloodstream. In healthy adults, the pathogens are usually destroyed by the immune system without any problems. In children whose immune system is not yet fully developed, as well as in seniors and adults with weakened immune systems, the elimination of the pathogens is not always successful.
These then reach the organs via the bloodstream and attack them. The result can be severe blood poisoning or septic shock, which leads to circulatory collapse. Both the sepsis and the shock it causes can be fatal for the patient. Chronic erythrasma can develop in diabetics.
This is a form of pseudomycosis that spreads in the body and fat folds of overweight people, and diabetes is particularly common. The infection manifests itself as scaly, brownish skin lesions that, if left untreated, can give off an unpleasant odor. Treatment with antibiotics is usually successful, but in some patients the disease does not heal. The erythrasma either does not go away completely or occurs again and again at short intervals.
When should you go to the doctor?
The typical skin changes indicate pseudomycosis, which must be examined by a doctor in any case. If you notice scaly or keratinized areas of skin in the groin, armpit or scrotum that hardly itch, a doctor is recommended. Patients at risk include people with obesity, diabetes mellitus, hyperhidrosis, and immunosuppression. Affected persons should consult their doctor if the symptoms mentioned occur and do not subside on their own within a week or even increase in intensity.
The pseudomycosis is treated by the family doctor or a dermatologist. You can also go to an internist with the complaints. If the condition has a very negative impact on well-being, therapeutic advice can be useful to accompany the medical treatment. The patient should talk to the doctor about the necessary measures and, if necessary, involve other medical professionals in the treatment. Children should be presented to the pediatrician when the reported symptoms appear and do not go away on their own.
Treatment & Therapy
The pathogen determines the treatment of a pseudomycosis. Nocardiosis is treated with antibiotics such as ceftriaxone in combination with aminoglycoside. In the case of actinomycoses, antibiotics in the form of aminopenicillin or tetracycline treatment are sufficient in the initial stage, although surgical interventions to open the abscess are required in the advanced stage of the disease.
Erythrasms are usually treated locally with miconazole and fusidic acid cream. Benzoic acid and ASA can also be given. Systemic therapy with erythromycin usually lasts two weeks and is associated with optimal healing prospects. One-dose therapy with clarithromycin is also possible in this variant of pseudomycosis.
Under certain circumstances, photodynamic therapy represents an alternative to pharmacological treatment. This treatment is carried out with red light and is usually combined with the drying of the skin areas involved using moisture-absorbing powder and air-permeable clothing.
In the case of pseudomycoses affecting the central nervous system, functional impairment can persist even after healing, which is usually countered with physiotherapeutic measures.
prevention
Since pseudomycoses caused by actinomyces often occur during dental operations, antibiotics are often given prophylactically before and after major dental operations. Since pseudomycoses specifically affect immunodeficient patients, strengthening the immune system is also a preventive step.
Aftercare
Pseudomycosis is caused by bacteria. The attending physician will therefore usually prescribe an antibiotic. Here the unconditional help of the patient is required. The antibiotic must be taken regularly and for a certain period of time so that it can develop its full effect. If the drug is stopped too early, complications or relapses can occur.
Diabetics and people who are very overweight often experience delayed wound healing. Sores in body folds are often very difficult to heal. Treatment with red light is recommended here. Corresponding devices are relatively inexpensive to purchase from retailers. Irradiation with red light dries out the affected areas of the skin and thereby intensifies the healing process. Medicinal powders also help absorb the moisture.
To avoid unnecessary sweating, loose, airy clothing made of natural materials should be worn during the infection. As with all infectious diseases, it is important to strengthen and stabilize the immune system. Vitamin-rich diet, exercise in the fresh air and moderate physical activity accelerate the healing process. A strengthened immune system helps older people and people with general immune deficiencies in particular to cope with pseudomycosis more quickly.
You can do that yourself
As pseudomycosis is caused by bacteria, the treating doctor usually prescribes an antibiotic. Good “compliance” is important here, which means that the patient should absolutely follow the doctor's instructions and take the prescribed antibiotic regularly. This is the only way to ensure the success of the treatment. The drug must never be discontinued prematurely, as this can lead to relapses or complications.
In the case of diabetics or people who are overweight, the sore spots may not heal. Mostly these are areas in skin or body folds. Additional treatments with red light devices are recommended here, as can be bought cheaply anywhere. Red light baths dry the affected areas of the skin, which contributes to faster healing. This effect can be enhanced with powders that absorb moisture. It is also advisable to wear natural, air-permeable clothing so that the affected areas of the body do not sweat unnecessarily.
A fresh, vitamin-rich diet, a regular daily routine and plenty of fresh air contribute to stabilizing the immune system and thus also to healing. This also applies to regular exercise and moderate sport. Older people in particular or people with general immune deficiencies benefit from an improved immune system because otherwise the pseudomycosis may not be able to completely heal in them.


.jpg)