Psoriatic arthritis is an inflammatory disease of the joints that is usually accompanied by psoriasis. About 5 to 15 percent of those affected by psoriasis develop this form of arthritis, the underlying cause of which has not yet been clarified.
What is psoriatic arthritis?

© Henrie - stock.adobe.com
As Psoriatic arthritis is an inflammatory disease of the joints, which manifests itself mainly in painful swellings in the joints of the hands and feet and the adjacent tendons.
Psoriatic arthritis or inflammatory joint disease is usually preceded by psoriasis. The most common form of this disease is so-called asymmetric psoriatic arthritis, in which the smaller joints of the hands and feet are affected differently in both halves of the body.
In addition, the so-called distal interphalangeal form of psoriatic arthritis primarily affects the end joints in the fingers and toes, which also often have changes in the nails.
causes
The underlying causes of a Psoriatic arthritis could not be conclusively clarified so far. A genetic predisposition (predisposition) is assumed, whereby certain triggering factors must also be present for the disease to manifest (outbreak).
These include febrile infectious diseases (angina tonsillaris, measles, bronchitis), hormonal changes during puberty or menopause as well as certain medications (ACE inhibitors, chloroquine) and psychological factors such as stress at work or in the family. The factors mentioned can not only contribute to the manifestation of the disease, but also trigger new flare-ups.
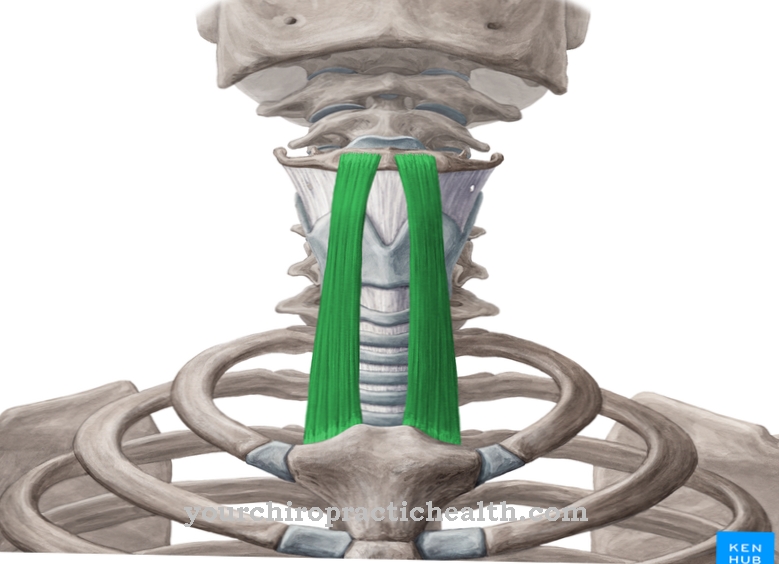
What is certain is that a dysregulation of the immune system (autoimmune processes) as a result of a bacterial infection can lead to the body's own structures such as the skin areas on joints being attacked. This triggers the inflammatory reactions characteristic of psoriatic arthritis, which can gradually expand to the underlying joints, their tendons, cartilage and bones.
Symptoms, ailments & signs
Psoriatic arthritis disease typically shows up in symptoms of both psoriasis (psoriasis) and arthritis (inflammation of the joints). There is redness, joint pain and swelling, mainly in the end joints of the fingers. Characteristic are the thickenings on the fingers, which are then colloquially referred to as sausage fingers.
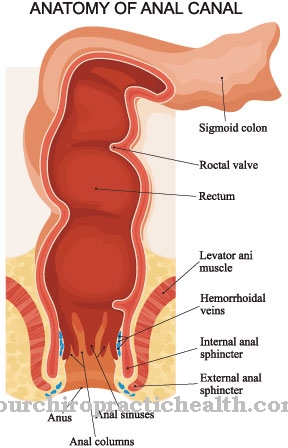
Your toes can also swell. In addition, inflammation of the tendon attachments is possible, for example on the Achilles tendon. Joint capsules and ligaments can also be affected. If this is the case, it leads to restricted mobility, deformation and pain. Eventually the joints may stiffen, initially mainly in the morning after long periods of rest.
Further symptoms are reddened, painful and sharply defined areas of the skin that are covered with a cuticle and itchy. They are known as psoriasis foci or plaques. They are most common on the kneecaps, below the elbow, or on the scalp. They can also develop in the gluteal fold.
The nails of the fingers and toes change; they deform, sometimes yellow and crumble. There are 3 types of the disease. In the common peripheral asymmetrical type, symptoms appear asymmetrically on the fingers and toes. In the peripheral symmetrical type, large joints on both halves of the body are affected. Finally, the axial type shows up in symptoms in the spine or sacroiliac joint.
Diagnosis & course
A Psoriatic arthritis is diagnosed on the basis of the typical symptoms, in particular on the basis of the painful swellings and skin changes on the affected joints. The diagnosis is confirmed by blood analyzes, which typically show elevated inflammation markers.
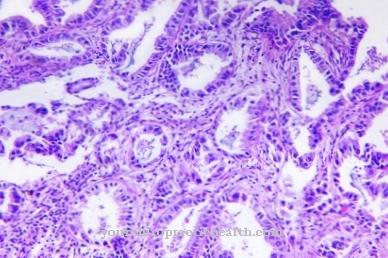
Skin samples and analyzes of the synovial fluid provide additional information about the clinical picture. In contrast to rheumatoid arthritis, in psoriatic arthritis the so-called rheumatoid factor (detection of specific antibodies that are characteristic of rheumatoid arthritis) can only be detected in isolated cases.
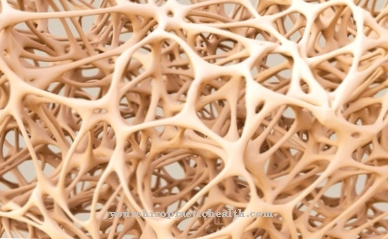
In the advanced stage of the disease, imaging methods such as X-ray (radiography) magnetic resonance tomography and sonography (ultrasound) allow statements to be made about existing changes in bones and joints. The course of psoriatic arthritis can vary greatly from person to person. For example, psoriatic arthritis can have a chronic or episodic, relapsing course.
Complications
Because of psoriatic arthritis, most people suffer from arthritis, which is also accompanied by psoriasis. As a result of these complaints, the quality of life of the patient is considerably restricted and also further reduced. Psoriatic arthritis can also lead to inferiority complexes or significantly reduced self-esteem if those affected are ashamed of the symptoms and no longer feel comfortable with their skin.
There are also various changes to the bones and joints of the person affected. In some cases, psoriatic arthritis can also lead to restricted mobility and difficulties in everyday life. Furthermore, the patients can also be dependent on the help of other people. Psoriatic arthritis is treated without complications. As a rule, drugs are used that can significantly alleviate and reduce the symptoms.
However, it cannot be universally predicted whether the course of the disease will be completely positive. Patients may then be dependent on lifelong therapy. Some drugs may also have side effects. The life expectancy of the person affected is usually not reduced by psoriatic arthritis.
When should you go to the doctor?
For psoriatic arthritis, a doctor should always be seen. The symptoms of psoriatic arthritis can only be completely alleviated through medical treatment, as this disease does not self-heal and in most cases the symptoms worsen significantly.
Early diagnosis and treatment always have a positive effect on the further course of the disease. The doctor should be consulted if the person concerned suffers from severe pain in the joints. A doctor should be consulted, especially in the case of persistent pain that occurs for no particular reason and reduces the quality of life of the person concerned. Reddening of the joints often indicates psoriatic arthritis and should be treated. Restrictions in movement and stiff joints can also indicate the disease. The nails on the toes and fingers can also change. Primarily, psoriatic arthritis can be diagnosed by a general practitioner or an orthopedic surgeon. Further treatment usually takes place by a specialist.
Treatment & Therapy
Because the cure is a Psoriatic arthritis has not been possible so far, the therapeutic measures aim to alleviate or reduce the respective symptoms. For this purpose, topical medication can be used for treatment, which is applied locally to the affected skin areas and joints.
Such a therapy is particularly useful in cases in which only individual joints are affected by psoriatic arthritis. In addition, systemic drugs such as non-steroidal anti-inflammatory drugs or NSAIDs such as acetylsalicylic acid, ibuprofen or ibuprofen are used as pain relievers and anti-inflammatory drugs. Photo therapy (light therapy) or bath therapy with salt water can also have a positive effect on the skin areas affected by psoriasis and alleviate the symptoms.
With the help of physiotherapeutic measures (physiotherapy, massages, heat and cold therapy), the mobility of the affected joints can be maintained or their stiffening slowed down. If the disease is at an advanced stage, a so-called basic therapy with long-term drugs such as methotrexate or sulfasalazine is indicated, in which the liver values of the person affected should be checked regularly.
Ciclosporin is used in some cases as an immunosuppressant to suppress the autoimmune reactions of the body's own defense system. In addition, so-called biologics or biologics (infliximab, etanercept, adalimumab) inhibit the tumor necrosis factor (TNF-alpha), which is held responsible for the inflammatory processes. On the other hand, because of the strong side effects, cortisones are only used in the presence of severe psoriatic arthritis.
prevention
As the underlying cause of a Psoriatic arthritis is not known, it cannot be specifically prevented. The manifestation of psoriatic arthritis can be prevented if necessary by avoiding trigger factors such as psychological stress and by early and consistent treatment of infectious diseases or hormonal changes.
Aftercare
Like psoriasis, psoriatic arthritis is also incurable. So there is no classic aftercare. Instead, those affected should lead a healthy lifestyle and avoid risk factors that could lead to relapses of the disease as much as possible. Regular exercise tailored to individual needs can have a positive effect on the course of psoriatic arthritis.
Sports that are gentle on the joints, such as swimming and cycling, are particularly recommended, but long walks in the fresh air are also beneficial for body and soul. As part of the aftercare, the attending physician can also prescribe physiotherapy so that the joints remain flexible. You may also be referred to a nutritionist, who can also reduce the risk of joint inflammation in order to ensure a healthy and balanced diet with a high proportion of fresh fruit and vegetables and whole grain products.
High-fat foods, ready meals and sweets, on the other hand, should rarely or never be on the menu. Furthermore, aids can make everyday life easier for those affected, which is why they should also be viewed as an important part of aftercare for psoriatic arthritis.
Gripping aids come into question as well as foam attachments for cutlery and cap openers, with which those affected can open bottles and glasses without any effort. Last but not least, in symptom-free phases it is advisable to have regular follow-up examinations with the attending physician so that he can document the course of the disease.
You can do that yourself
Since this painful disease is often caused by a dysregulation of the immune system, patients are urgently advised to lead a healthy lifestyle. This includes a regulated sleep-wake cycle as well as a diet rich in vital substances and fiber with little fat and sugar. Existing excess weight should be reduced, especially if the knee joints, toes or Achilles tendons are affected. Less weight relieves the joints, joint capsules and ligaments.
Because of the medication to be taken for psoriatic arthritis, patients should take care of their liver and avoid alcohol and nicotine. At the same time, those affected should drink a lot so that the body can better flush out toxins. Patients should also exercise as much as possible. Those who can no longer walk or cycle should switch to water sports such as aqua jogging or water aerobics. The aim is to maintain the mobility of the individual joints. Massages, physiotherapy and / or warm or cold therapies have also proven to be helpful.
If the symptoms lead to a lower self-esteem because the patients literally do not feel comfortable in their own skin, then psychotherapeutic treatment is advisable. But contact and exchange with other patients also help. Various self-help organizations provide these contacts as well as further information about the disease, for example the Psoriasis Association (www.psoriasis-bund.de), the Psoriasis Info (www.schuppenflechte-info.de) and the Rheuma League (www.rheuma -liga.de).



.jpg)
.jpg)

.jpg)





.jpg)





.jpg)