Under pulmonary hypertension or. Pulmonary hypertension is understood to mean an increase in the mean pressure of the pulmonary artery (pulmonary artery) to over 20 mmHg. In most cases, pulmonary hypertension occurs as a secondary complication of a primary underlying disease.
What is Pulmonary Hypertension?

© elvira fair - stock.adobe.com
As pulmonary hypertension (also pulmonary arterial hypertension or pulmonary high pressure) is a disease that is associated with an increase in the mean pulmonary artery pressure (to more than 20 mmHg at rest) and vascular resistance and, in many cases, leads to right heart failure.
Characteristic symptoms of pulmonary hypertension are severely restricted performance, shortness of breath, fatigue, circulatory disorders, angina pectoris, peripheral edema (water retention), cyanosis (blue discoloration of the skin) and Raynaud's syndrome (reduced blood flow to toes and fingers).
In principle, a distinction is made between chronic and acute pulmonary hypertension. While acute pulmonary hypertension is characterized by a temporary constriction of the vessels in the pulmonary circulation, for example as a result of overload, chronic pulmonary hypertension leads in the long term to hypertrophy (increase in size) of the pulmonary vascular muscles, which later develop into connective tissue, and thus to sclerosis (hardening) as well a loss of elasticity of the vessels. At this stage of pulmonary hypertension, oxygen uptake is permanently and irreversibly difficult.
causes
A pulmonary hypertension often correlates with various underlying diseases.
In many cases, pulmonary hypertension is due to primary diseases such as chronic obstructive pulmonary disease (COPD) as a result of heavy nicotine consumption, pulmonary emphysema, pulmonary fibrosis, iterative lung (micro) embolism (sudden pulmonary artery occlusion), asthma, AIDS, sleep apnea syndrome (respiratory arrest during sleep), Sickle cell anemia or congenital heart defects (secondary pulmonary hypertension).
In rare cases, pulmonary hypertension occurs as an autonomic disease, although the specific cause usually remains unexplained (idiopathic or primary pulmonary hypertension).
It is known, however, that those affected by primary pulmonary hypertension increasingly secrete certain vasoconstrictors (substances that constrict blood vessels) such as endothelin or thromboxane and / or have an increased serotonin level, while at the same time a reduced synthesis of prostacyclin and nitric oxide can be observed. In addition, pulmonary hypertension can also be medically induced in certain people.
Symptoms, ailments & signs
Pulmonary hypertension does not always start with symptoms. Eventually, as the disease progresses, there will be clear signs of a serious illness. The lack of oxygen in the lungs initially leads to a decrease in physical and mental performance. Pulmonary hypertension also leads to fatigue, fatigue and listlessness.
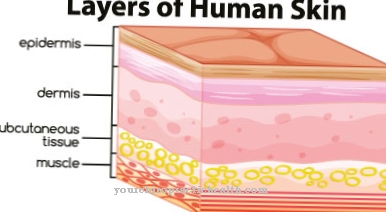
People feel limp and have unusual chest pain or swelling in their legs. Externally, there is also bluish discoloration of the skin and lips, combined with numbness and cold feelings in the limbs. The lack of oxygen supply can cause circulatory problems such as dizziness, circulatory disorders and palpitations.
As the disease progresses, cardiac arrhythmias develop. These are occasionally noticeable in the form of a heart attack or reduced performance. Due to the increasing stress on the heart, a right heart weakness can develop, which reduces life expectancy and usually also restricts the quality of life.
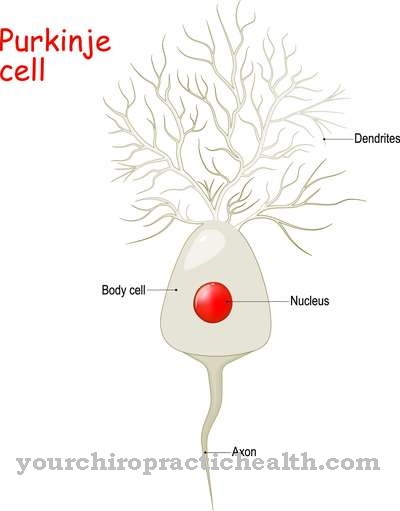
If the pulmonary hypertension continues to progress, the patient can die from it. There is a risk of organ damage and heart attacks. In general, pulmonary hypertension favors the development of various diseases. Strokes, osteoarthritis, ulcers and neurological disorders can then occur, which are also associated with symptoms and complaints.
Diagnosis & course

An X-ray examination of the chest (chest X-ray) allows first indications of a pulmonary hypertension. The diagnosis is confirmed by a cardiac catheter examination or Doppler echocardiography, during which the pulmonary arterial blood pressure can be determined.
A value of 25 mmHg or more is referred to as manifest and between 21 and 24 mmHg as latent pulmonary hypertension. An increased BNP value (brain natriuretic peptide or natriuretic peptide type B) in the serum indicates additional heart failure. The resilience of the individually affected person can be recorded with a 6-minute walk test by measuring the pulmonary pressure. The prognosis for pulmonary hypertension is usually poor.
If the pulmonary hypertension is more than 30 mmHg, the five-year survival rate is only 30 percent and worsens if the right heart failure goes wrong. If untreated, pulmonary hypertension has a three-year life expectancy based on findings.
Complications
Pulmonary or pulmonary arterial hypertension (PAH) is divided into five different classes, depending on the cause of the disease. What all five classes have in common is that, if left untreated, the disease leads to considerable complications and symptoms, which are usually not reversible. An early diagnosis with the consequence of an early targeted therapy of the triggering underlying disease offers the best chance of a cure.
The PAHs described as primary or idiopathic, for which no triggering factors are found, have in common that pulmonary hypertension is usually accompanied by an increased concentration of vasoconstrictors with a simultaneous decrease in the concentration of hormones that cause the vessels to widen (vasodilation). If the symptoms of primary or idiopathic PAH are not treated successfully, serious complications gradually set in, the progression of which also depends on the severity of the pulmonary hypertension.
Arterial pulmonary blood pressure values above 25 mm Hg correspond to a manifest PAH with a poor prognosis. Pressure values in the range of 21 and 24 mm HG are latent pulmonary hypertension. If right heart failure, which is often observed in these cases, is added as a complication, the prognosis for survival is unfavorable unless the path to a heart-lung transplant is open.
Heart failure is noticeable not only through a clearly noticeable drop in performance, but also through certain laboratory values. Elevated BNP values (Brain Natriuretic Peptides) are classified as an indicator of heart failure.
When should you go to the doctor?
This type of pulmonary should always be treated by a doctor. If left untreated, various complications can occur which, in the worst case, can be fatal for those affected. An early treatment of this type of pulmonary always has a very positive effect on the further course of the disease. A doctor should then be consulted if the person concerned has clear symptoms of an insufficient supply of oxygen. The skin can turn blue, and the person concerned has to breathe quickly and becomes tired.
Exhausting activities can no longer be carried out without further ado. Furthermore, disturbances of the blood circulation indicate these pulmonals and must be examined if they do not go away on their own. Those affected often also suffer from dizziness or from numbness all over their body. The risk of strokes is also significantly increased, so that the person affected is dependent on regular examinations.
First and foremost, the pulmonary can be recognized by a general practitioner. Further treatment, however, always depends on the exact severity of the symptoms and is carried out by a specialist. This may also limit the patient's life expectancy.
Treatment & Therapy
The therapeutic measures are aimed at one pulmonary hypertension in most cases to the treatment of the underlying disease. In addition, depending on the stage, the disease is treated with medication.
The endothelin receptor antagonist bosentan or the prostacyclin analogue epoprostenol are recommended for stage III pulmonary hypertension. In some cases, sildenafil (PDE-5 inhibitor), iloprost (prostacyclin analogue) as well as treprostinil and beraprost are also used. If the disease is already stage IV, epoprostenol is used primarily, followed by bosentan, treprostinil, alpostadil and intravenous iloprost.
If the vasoreactivity test is positive (response to vasodilating nitric oxide), calcium channel blockers such as diltiazem or nifedipine can be used. If necessary, if there is no response to conservative measures, an atrioseptostomy, in which an artificial connection is established between the two atria of the heart, may be indicated. If pulmonary hypertension is already manifest, treatment can usually only be palliative (alleviation of the symptoms) or as part of a transplant (lung or heart-lung transplant).
For this reason, children with a congenital heart defect are operated on as early as possible to prevent the development of pulmonary hypertension. To avoid intracardiac thrombosis, an additional anticoagulation (blood coagulation inhibition) is indicated. In some cases, long-term oxygen therapy is also used to relieve symptoms, while diuretics and digitalis are used to treat right heart failure. In addition, in the presence of pulmonary hypertension, smoking cessation and weight reduction in the case of overweight are recommended.
prevention
One pulmonary hypertension can be prevented to a limited extent. Consistent therapy of underlying diseases that can cause pulmonary hypertension reduces the risk of a manifestation. Refraining from nicotine consumption can also prevent chronic obstructive pulmonary diseases and, accordingly, pulmonary hypertension.
Aftercare
In pulmonary hypertension, both causal and symptomatic follow-up care is provided. Causal follow-up care is important to avoid the disease becoming chronic. If chronic pulmonary hypertension occurs, only symptomatic treatment is possible. In some cases, a lung or heart transplant may be necessary.
Oxygen therapy is advisable due to the high lung pressure and lack of oxygen. This helps to alleviate the symptoms and improve the quality of life for those affected. In addition, the pulmonary vascular resistance is lowered with the help of drugs. For this purpose, active substances that dilate blood vessels, such as phosphodiesterase inhibitors, are used.
Medicines to support the weakened heart are also prescribed. Diuretics or digitalis preparations are used here. After the illness, vigorous physical activity should be avoided as this represents a risk factor for further damage to the heart or lungs. Furthermore, a healthy diet in combination with light training under professional guidance is important.
Other approaches should include giving up nicotine and alcohol, and avoiding obesity. Check-ups at regular intervals by a specialist are essential. These focus on checking lung and heart failure and adjusting medication if necessary. The prognosis for pulmonary hypertension tends to be negative, but depends on various factors such as the triggering cause and the ability of the heart to adapt to the increased pressure.
You can do that yourself
First of all, the affected patients have to find out with their doctor how pulmonary hypertension or pulmonary hypertension came about. If there are underlying diseases that led to pulmonary hypertension, they must be treated. If the pulmonary hypertension is medicated, the medication should be changed.
In any case, it is important to take this disease and its symptoms seriously, otherwise pulmonary hypertension has a poor prognosis. The medication prescribed by the doctor must be taken. Smoking is taboo for patients with pulmonary hypertension. If possible, they should move to rural areas with less particulate matter. The use of fine dust filters in the home can also bring relief to those affected.
Since patients with pulmonary hypertension are prone to thromboembolism, they should be shown vein exercises that can prevent thrombosis. Alternating showers and treading water are also recommended measures. In addition, patients should not stand or sit for too long, but instead move as much as possible within their capabilities. A sufficient supply of fluids in the form of two to three liters of water or herbal tea a day is recommended. The mineral water should contain little sodium.
Further help for self-help is also provided by self-help groups that are listed in the pulmonary high pressure information center (www.lungenhochdruck-infocenter.de/services/selbsthilfegruppen.html).

.jpg)


.jpg)


.jpg)


.jpg)




.jpg)