The Reflux esophagitis is a disease that has been increasing in recent years. According to statistics, at least 10% of the population in industrialized countries suffer from this form of esophagitis.
What is reflux esophagitis?

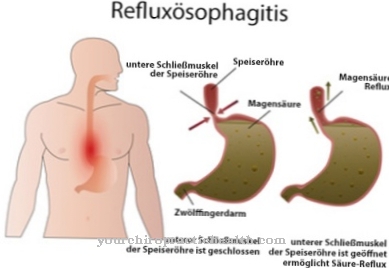
At a Reflux esophagitis the mucous membrane in the lower part of the esophagus is inflamed. This inflammation is caused by the backflow (reflux) of digestive juices from the stomach into the gullet (esophagus).
If hydrochloric acid, pepsin or bile acids act on the esophagus for a long time, they irritate and damage its mucous membrane. In 65% of those affected, no signs of inflammation are detected during an endoscopy, despite severe and agonizing symptoms. This type of reflux esophagitis is known as "non-erosive reflux esophagitis" (NERD). "Erosive" here refers to a visible, superficial and inflammatory change in the esophageal lining.
35% of patients suffer from "erosive reflux esophagitis" (GERD). During an endoscopy, clear signs of inflammation can be seen. Reflux esophagitis is also referred to as reflux disease.
causes
The presumed causes of the Reflux esophagitis in principle only refer to the reasons that lead to an increased reflux of gastric acids etc.
It is not yet known why this ultimately leads to inflammation of the esophagus in some people and not in others. These causes are divided into direct (primary) and indirect (secondary) causes and influence the closure mechanisms of the esophagus and the stomach. The undulating transport movement of the esophageal muscles (peristalsis) can also be affected.
The direct causes include certain foods such as fats, stimulants such as alcohol or irritating food components such as caffeine, tea and peppermint. In addition, there are changes in the hormonal level, such as can occur during pregnancy. Psychological stress, age-related muscular weaknesses, changes in the pressure conditions in the abdomen due to constipation, pregnancy, etc.
The secondary causes of reflux esophagitis are based on other diseases, such as abnormal or operative changes at the stomach entrance or operative damage to the lower esophageal sphincter (a type of sphincter). In premature births, this muscle is often not yet properly developed. Chronic, inflammatory diseases such as scleroderma or nerve diseases due to diabetes are also indirect causes of reflux esophagitis.
In general, being overweight or having a diaphragmatic hernia, which causes part of the stomach to protrude, are risk factors.
Symptoms, ailments & signs
The main symptom of the disease is heartburn, a burning pain behind the breastbone and in the upper abdomen. It feels like something sharp is flaring up in the stomach area and esophagus. In addition, there is a feeling of pressure and heat in the chest, which is often wrongly associated with diseases of the heart.
Heartburn occurs initially after meals and later without food. It increases when you lie down or when you stoop. In addition, those affected often feel sour and air and stomach acid rise up into the mouth. Bad breath develops.
Constant contact with acid causes the esophageal lining to become irritated and inflamed. This manifests itself in difficulty swallowing and pain in the throat. For some patients, the throat feels extremely dry, but drinking too much does not get rid of this feeling of dryness.
For others, the inflammation makes them feel like they have something stuck in their throat, which leads to constant clearing of throat and irritable cough at night. Hoarseness can also occur. Patients often eat less because of difficulty swallowing and pain in the esophagus. If the disease persists, weight loss can occur. If left untreated, the inflammation can spread to the larynx and lungs.
Diagnosis & course
Diagnosing a Reflux esophagitis is done through an esophagoscopy, an examination of the esophagus with the help of a camera tube, and a gastroscopy, a reflection of the stomach.
If changes in the mucous membrane become visible, they enable the disease to be classified. In addition, there is the option of taking a small tissue sample during these examinations. A 24-hour acid measurement, a pH-metry, is carried out and allows statements to be made about the duration and strength of the acid reflux within a day.
The esophagus manometry, a muscle function measurement, is rarely performed these days. Reflux esophagitis leads to beret esophagus in a small number of cases.
The mucous membrane of the esophagus changes, its structure resembles that of the gastric mucosa. This altered mucous membrane can lead to ulcers or esophageal cancer.
Complications
The symptoms of reflux esophagitis are very uncomfortable and can lead to serious complications. Because of this, this condition needs to be diagnosed and treated early. Those affected suffer primarily from severe heartburn. Heartburn itself mainly occurs after eating acidic or salty foods and has a very negative effect on the quality of life of the person affected.
Persistent belching or strong coughing can also emerge due to the illness. In severe cases, patients experience shortness of breath. If the disease is not treated, in the worst case it can lead to the formation of ulcers and furthermore to cancer in the esophagus. This can also lead to patient death. In most cases, reflux esophagitis can be treated with medication.
There are no particular complications or other complaints. Heartburn in particular can be relieved. Furthermore, many sufferers are dependent on surgical interventions, which can relieve the symptoms permanently and limit the acid production of the stomach.
When should you go to the doctor?
Reflux esophagitis should usually always be treated by a doctor. This disease does not self-heal and in most cases the symptoms worsen. In the worst case, reflux esophagitis leads to inflammation of the esophagus, which can lead to further complications. A doctor should then be seen if the person concerned suffers from severe heartburn. Heartburn can occur sporadically or after eating various meals and have a negative impact on the quality of life of the person affected.
Furthermore, a strong bad breath in the affected person can indicate reflux esophagitis. The patients often have pain in the throat or even difficulty swallowing, which can lead to coughing or hoarseness. Furthermore, the patient's larynx can become inflamed. Reflux esophagitis can be treated by a general practitioner or an internist. As a rule, there are no particular complications.
Treatment & Therapy
Treating a Reflux esophagitis takes place conservatively or surgically. In most cases, conservative treatment using certain drugs is sufficient.
Proton pump inhibitors reduce the acidity of the stomach's contents by not making as much hydrochloric acid in the stomach. Antacids do not interfere with acid production, but neutralize the existing acid content. Prokinetics have a supportive effect, as they increase the closing force of the lower esophageal sphincter and have a promoting effect on the emptying of the stomach. Conservative therapy must be carried out for life, as reflux esophagitis recurs after the medication is discontinued.
In the rare cases in which conservative treatment is unsuccessful, a surgical procedure, a "fundoplication", can be performed. The upper part of the stomach is placed like a cuff over the lower esophageal sphincter and thus has a reinforcing effect on the occlusion of the esophagus.
You can find your medication here
➔ Medication for heartburn and bloatingprevention
Preventive measures include weight loss, smaller, more frequent meals, and avoiding too fatty or irritating foods on the Reflux esophagitis act. Sleeping with your upper body elevated, wearing loose clothing, avoiding stress and excessive alcohol consumption also have preventive effects.
Aftercare
Follow-up care for reflux esophagitis is varied and very individual. Above all, the removal of the cause of the reflux should be given priority. Often this cannot be done adequately. In reflux esophagitis, long-term or even lifelong therapy with gastric acid reducers is required.
Follow-up care here primarily relates to the alleviation and ultimately suppression and healing of the esophagitis by preventing stomach acid from flowing back into the esophagus. As a rule, this can only be treated with medication or even surgically. The specialist, a gastroenterologist, monitors the course of treatment and the severity of the disease.
Follow-up care here is primarily based on regular check-ups. Since the disease is individual and can have various causes, as well as operative consequences, there is no uniform follow-up care and no clearly definable statement about the course and healing. Reflux esophagitis needs long-term treatment, especially if the patient's symptoms persist.
If the stomach does not close properly, reflux can occur even with certain positions, which irritates the esophagus again and causes the reflux esophagitis to flare up. Individual advice and treatment for the patient is essential here.
You can do that yourself
There are many things the patient can do themselves to prevent reflux esophagitis. On the one hand, there is a change in diet. If possible, spicy foods should not be consumed as they can worsen the symptoms of reflux oesophagitis. You should also avoid hot or sour food.
The patient should also avoid alcohol or coffee (or caffeine in general) during this period, as they can cause gastric acid reflux, which is the main cause of reflux esophagitis. As a countermeasure, soothing substances can also be eaten or drunk. Chamomile tea, for example, can be helpful here.
In order to lower the pH of the stomach acid and thus the aggressiveness of the stomach acid, the patient can take medication in the form of proton pump inhibitors such as omeprazole or pantoprazole. Drugs that reduce inflammation, such as ibuprofen or paracetamol, can also be helpful. A positive side effect of the medication is the alleviation of pain that can be caused by reflux oesophagitis.
If the patient continues to notice symptoms, such as stabbing pain behind the breastbone or more frequent belching, which indicates worsening symptoms, the patient should consult a doctor who may prescribe an endoscopy. In general, the patient should see a doctor for regular check-ups, since reflux esophagitis can be a precursor to aggressive esophageal cancer.

.jpg)