As Rectocele is a bulging of the front wall of the rectum into the vagina. It is often associated with a lowering of the pelvic floor.
What is a rectocele?

© pixdesign123 - stock.adobe.com
From one Rectocele is the talk when a bulging of the rectum occurs. There is a protrusion into the female vagina directly above the sphincter muscles.
In most cases, the rectocele bulges towards the vagina or urinary bladder. Only women are affected by it. The sac is associated with the general sinking of the lower intestines. The pelvic floor gives way under pressure.
In addition, there are disturbances in defecation.
A rectocele is found in around 50 percent of all women over 50 years of age. However, therapy only takes place if those affected are suffering from symptoms.
causes
The causes for the development of a rectocele have not yet been fully clarified. It is not uncommon for those affected to suffer from sagging or insufficiency of the pelvic floor, which results in changes in the normal anatomy. Some risk factors are known that can promote the occurrence of a rectocele.
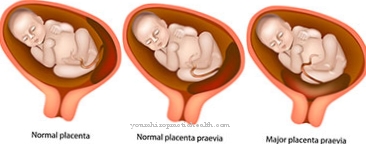
These include pregnancies, natural births, chronic constipation, gynecological surgery, old age, obesity and considerable pressing movements when defecating. Due to anatomical requirements, a rectocele only occurs in women. The male sphincter muscles are equally pronounced, while in women the external sphincter muscle on the front is increasingly thinned.
In addition, the man's prostate (prostate gland) allows the intestines to expand forward. However, women do not have such anatomical obstacles. As a result of multiple births and the weakening of the connective tissue, the pelvic floor can shift in the lower direction with increasing age. In this way, there is enough space under the bony ring for the rectum to expand and expand without resistance.
Symptoms, ailments & signs
If the rectocele takes on a certain size, this causes severe problems with the defecation. For this reason, rectoceles are a common trigger for Obstructive Defecation Syndrome (ODS). If a woman has been constipated for several years, the changes are hardly noticed by her, as they progress only slowly.
Typical complaints with a rectocele are strong and long pressing when defecating, eczema, itching, the appearance of blood or mucus when defecating, pain in the rectum or perineal region and the passing of the bowel movement in several sections. It is not uncommon for patients to have to resort to laxatives in order to defecate at all. Occasionally, ulcers within the rectum also appear, which doctors call solitary rectal ulcer.
The symptoms can be so intense that they significantly impair the quality of life of the women concerned. They are caused by the fact that the rectocele is filled with stool before emptying. If there is also a subsidence of the pelvic floor, the angle of the rectum and anus changes. When pressing, the pressure is therefore not directed to the anus, but to the rectocele.
The rectocele wall is so thinned that it no longer has functional muscles. The rectum wall is longer in the anterior direction. In the case of an empty rectum, wrinkles form that fall down towards the anus. This incident is known in medicine as rectal prolapse.
Diagnosis & course of disease
The diagnosis of a rectocele is difficult and time-consuming, as it and its symptoms often take years to develop. First, the patient's medical history is created. The doctor will then do a physical exam, which usually reveals a subsidence of the perineum. A sphincter weakness is often detected as part of a digital palpation.
Another examination option is endoscopy, which consists of rectoscopy or proctoscopy. Sometimes further examinations are carried out, such as a colonoscopy to clarify constipation or gynecological examinations. Defecography is the key to diagnosing a rectocele.
With this procedure, the rectocele can be visualized with the help of a contrast agent when defecating. A rectocele does not always cause symptoms. However, in the case of larger bulges, there may be problems with drainage, so that medical treatment is required.
Complications
Rectoceles very often do not cause any symptoms and therefore often do not require treatment. However, larger rectoceles can lead to complaints and complications that require at least conservative treatment or, in rare cases, surgical intervention. Older women in particular or women who have had multiple pregnancies, including overweight women, are more likely to have a larger rectocele.
The so-called obstructive defecation syndrome can occur as a complication in these cases. In this syndrome, chronic constipation is at the fore. The affected women suffer from a constant urge to defecate, which is associated with the stubborn feeling of incomplete emptying. In addition to abdominal pain, constant discomfort and nausea, stool incontinence can develop over time.
Furthermore, larger rectoceles are often characterized by excruciating itching and eczema in the anus area. There is often pain in the perineum area, with the hard-pressed stool covered with blood and mucus. Sometimes ulcers even develop in the rectum, also known as rectal ulcers.
The quality of life of women can be so impaired that psychological problems can arise. Some women suffer from depression or other mental illnesses due to their chronic complaints. In rare cases, the symptoms can become so severe that an operation is necessary. The operational risks depend on the extent of the surgical intervention required.
When should you go to the doctor?
A rectocele should always be treated by a doctor. Further complications can only be avoided through medical treatment. This disease does not heal itself. The doctor must be consulted for the rectocele if the person concerned has been constipated for several years. The constipation can be sporadic or chronic. If these symptoms are present, medical treatment is necessary. Furthermore, the anus may itch after defecation, as the person concerned has to press hard when defecating.
In some cases, patients also resort to laxatives to relieve the discomfort of the rectocele. If these symptoms occur over a longer period of time and do not heal on their own, a doctor must be consulted. The rectocele is treated by an internist, proctologist or a general practitioner. Further treatment depends heavily on the exact severity of the symptoms.
Therapy & Treatment
Usually a rectocele is initially treated in a conservative way. The patient's diet is changed. She is also given stool-softening drugs. The patient also receives preparations that increase the speed of the intestinal transport. Physiotherapeutic measures take place when the pelvic floor muscles are weakened or there are coordination problems.
If complications such as ulcers, a herniated rectum or bleeding occur, or if the rectocele becomes large, surgery is usually required. Surgical methods that can be considered are the S.T.A.R.R.operation or a rear vaginal tightening. As part of the S.T.A.R.R. procedure, the surgeon removes a cuff from the rectum four to eight centimeters wide above the anus.
In posterior colporrhapy, it strengthens the area between the rectum and vagina and the posterior vaginal wall, which counteracts any further expansion of the rectocele.
prevention
To avoid a rectocele in the first place, women are recommended to consistently undergo postpartum regression and pelvic floor exercises. Exercising the anal sphincter should also be considered.
Aftercare
Follow-up care for a rectocele depends on how the condition progresses. A small rectocele doesn't always need treatment. A one-time follow-up examination is usually sufficient. If the patient does not show any unusual symptoms, no further action is required. In individual cases, injection treatment takes place and the family doctor must ask as part of the follow-up care whether the patient is experiencing side effects or medical complications.
After an operation, as it is necessary for a lengthy rectocele, there is usually a short stay in hospital. The chief physician checks the surgical wound and takes an anamnesis. The prescribed medication may have to be reset or discontinued. Even with a surgical procedure, the further procedure depends on the course.
In the event of an operation, follow-up care is provided by the responsible chief physician. Usually, the patient's in-house gynecologist is also included in the follow-up care. If the rectocele goes well, the patient can be discharged. The doctor will explain any risks to you and ask you to have regular routine examinations. Further follow-up care is usually not necessary for a fully recovered rectocele.
You can do that yourself
The rectocele can be relieved of its disturbing symptoms to a limited extent with self-help. This applies in particular to defecation, which is often hindered by the sack-like protuberance when pressing. The extent to which self-help is possible and what this looks like is best discussed with the treating doctor or a specialized physiotherapist.
Defecation is an important issue for patients when it comes to rectocele. Here it is important to take specific measures to facilitate bowel movements. In particular, strong pressing should be avoided as this intensifies the rectocele and makes bowel movements particularly difficult. Constipation is therefore particularly a nuisance in rectocele. Therefore, stool regulation is very important as a self-help. This can be achieved through a diet rich in fiber and a sufficient amount of water. Exercise is also helpful as it can naturally stimulate bowel movements. If these measures are not enough, psyllium preparations are helpful. This should only be taken after consulting the attending physician.
The rectocele can also be influenced somewhat with pelvic floor training and training of the vaginal muscles. The exercises can be learned by physiotherapists and gynecologists and are designed for regular use at home. In general, bowel movements should only last a short time, long sitting on the toilet intensifies the symptoms. Patients would rather go to the toilet again later than induce a bowel movement by pressing hard.


.jpg)



















.jpg)



