Renin is an enzyme with a hormone-like effect. It is made in the kidney and plays a role in regulating blood pressure.
What is renin
The name Renin is derived from the Latin "ren" for kidney. It is an enzyme that has a hormone-like effect. Renin is produced in the kidneys of vertebrates. Renin is released when the blood pressure is low.
Catecholamines can also increase the release of renin. However, key stimuli for the secretion of renin are always associated with a drop in blood pressure. Renin is the initiator of the Renin-Angiotensin-Aldosterone System (RAAS). This is used to increase blood pressure. Renin was discovered in 1898 by the Finnish physiologist Robert Adolph Armand Tigerstedt.
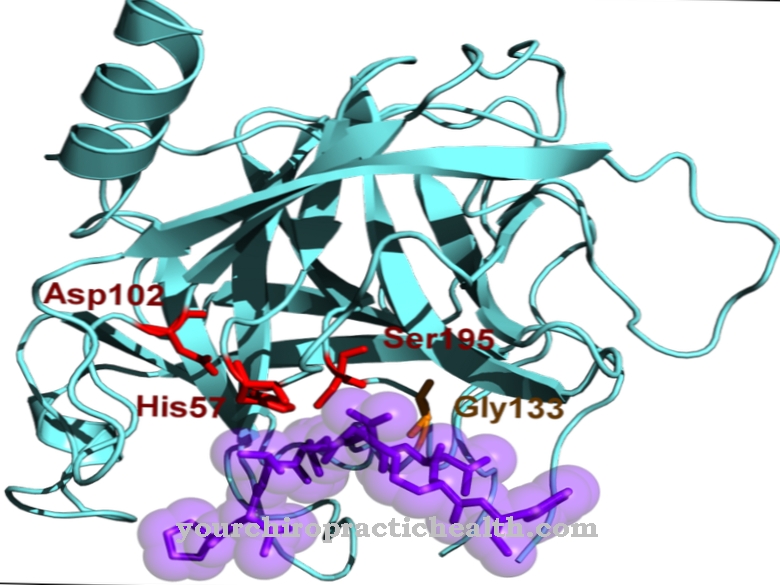
The enzyme renin consists of two lobes. Between these two lobes there is a gap that contains the active center of the enzyme with two catalytic aspartate groups. The inactive precursor of renin is also known as prorenin. It is also equipped with an N-terminal propeptide. The concentration of prorenin in the blood plasma is a hundred times higher than that of renin.
Function, effect & tasks
Renin is an important part of the renin-angiotensin-aldosterone system. The RAAS is a regulated circuit that is formed by various enzymes and hormones and controls the water and electrolyte balance in the body. The RAAS is one of the most important measures of the body to regulate blood pressure.
The renin-angiotensin-aldosterone cascade begins with the release of the enzyme renin. The enzyme is produced in the juxtaglomerular apparatus of the kidney. This consists of specialized connective tissue and blood vessel cells and the macula densa. Specialized cells of the urinary tubules are found in the macula densa. The task of the juxtaglomerular apparatus is to measure the blood pressure in the kidney's blood vessel. At the same time, it also measures the salt content in the urinary canals and reacts to signals and stimuli from the vegetative nervous system. Various hormones also influence the functioning of the juxtaglomerular apparatus. When the juxtaglomerular apparatus detects reduced blood flow to the kidney corpuscles, more renin is released.
Renin is also released when the baroreceptors, the blood pressure sensors of the vas afferens, measure decreased blood pressure. An increased release of renin is also initiated when the amount of fluid in the kidney corpuscles decreases. The decrease in the glomerular filtration rate (GFR) leads to increased secretion as well as a decreased concentration of saline ions in the urine. The salt sensors in the macula densa of the juxtaglomerular apparatus are responsible for the measurement. In summary, renin is always released when blood pressure drops and / or when there is a threat of a loss of table salt and water.
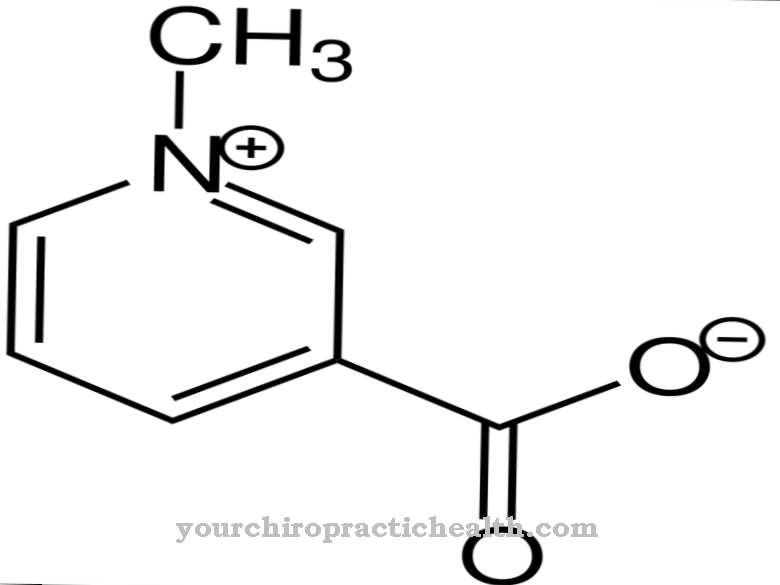
Renin has a protein-splitting effect and splits the protein angiotensinogen produced in the liver. This is how angiotensin I is produced. It is converted into angiotensin II by the angiotensin converting enzyme (ACE). Angiotensin II is the end product of the renin-angiotensin-aldosterone cascade. It causes small blood vessels to narrow. This increases blood pressure. Angiotensin II also releases aldosterone in the adrenal cortex. Aldosterone is a hormone that promotes the reabsorption of water and sodium in the kidney. This mechanism also increases blood pressure.
Education, occurrence, properties & optimal values
Renin is mainly produced in the cells of the juxtaglomerular apparatus. The precursors required for this are modified in the endoplasmic reticulum and in the Golgi apparatus of the renin-producing cells after translation. But renin is not only synthesized in the kidneys, but also in a number of other organs.
The extrarenal production sites of renin include the uterus, adrenal glands, pituitary gland, central nervous system, and salivary glands. However, the main production takes place in the kidneys. The renin value is determined in the blood plasma. Normal values for lying adults are 2.90-27.60 pg / ml. For standing adults, the normal values increase to 4.10-44.70 pg / ml.
Diseases & Disorders
An unnaturally high renin value arises, for example, from a low sodium intake, from low blood pressure or from a lack of fluids. Laxatives, diuretics, and some hormonal contraceptives also increase blood renin levels.
If there is an overproduction of aldosterone (primary hyperaldosteronism), however, the renin level may be lowered. Unnaturally low values occur in patients with diabetes mellitus or with a very high sodium intake.
Renin also plays an important role in the development of high blood pressure (hypertension). In many cases, the high blood pressure is caused by a narrowing of the renal arteries called renal artery stenosis. This stenosis is usually caused by arteriosclerosis. Cholesterol breakdown products and other substances are stored in the vessel wall. This thickens, so that the blood in the affected vessels can flow much more poorly. Renal hypertension develops as part of renal artery stenosis. This is triggered by the gold leaf mechanism.
The gold leaf mechanism ensures that renin is released and the renin-angiotensin-aldosterone system is activated in the event of a reduced blood flow to the kidneys. The increase in renal water and salt retention and the constriction of the vessels (vasoconstriction) increases blood pressure. This creates arterial hypertension. However, renal high blood pressure usually only develops when the renal artery is more than 75 percent blocked.
With a minor narrowing of the kidney vessels, the patient may be symptom-free. A renin-producing tumor can also lead to high blood pressure by activating the RAAS. The same is true of renal cell carcinoma, chronic pyelonephritis, cystic kidneys and glomerulonephritis.



.jpg)





.jpg)



.jpg)










.jpg)
