As Rifampicin is called an antibiotic.It comes from the fungus Streptomyces mediterranei.
What is rifampicin?

Rifampicin is one of the antibiotics and belongs to the group of rifamycins. It can be used against different types of bacteria. Rifampicin is considered to be particularly effective in the treatment of tuberculosis, against which it is used together with other drugs.
In 1957 the first isolation of the substance from the fungus Streptomyces mediterranei took place. They develop an antibacterial effect. Rifampicin became the most efficient representative of these substances. The antibiotic is produced semi-synthetically from rifamycin B. This substance is in turn taken from the bacterial genus Amycolatopsis rifamycina.
Rifampicin is primarily used to treat mycobacterial infections. In addition to tuberculosis, this also includes leprosy. In addition, the antibiotic is suitable for combating staphylococci, which are resistant to methicillin. Furthermore, it develops its effect against Legionella pneumophila and against enterococci.
Pharmacological effect
Rifampicin's mode of action is based on its binding to the bacterial enzyme RNA polymerase. This enzyme is urgently needed by bacteria for the production of essential proteins. As they no longer receive this vital protein, the bacteria die as a result.
With its effect, rifampicin captures both bacteria inside the cells and germs that are outside. The antibiotic works best in an alkaline or neutral environment. This mainly exists outside the cells. In contrast, the positive effect in the acidic area within the cells or in cheesy tissue is lower.
Rifampicin has the ability to kill bacteria. The antibiotic is not only effective against mycobacteria, but also against gram-positive, gram-negative and atypical bacteria. These include, for example, Staphylococcus epidermidis, Staphylococcus aureus, Streptococcus viridans, Streptococcus pneumoniae, Haemophilus influenzae, Neisseria meningitidis and Coxiella burnetii.
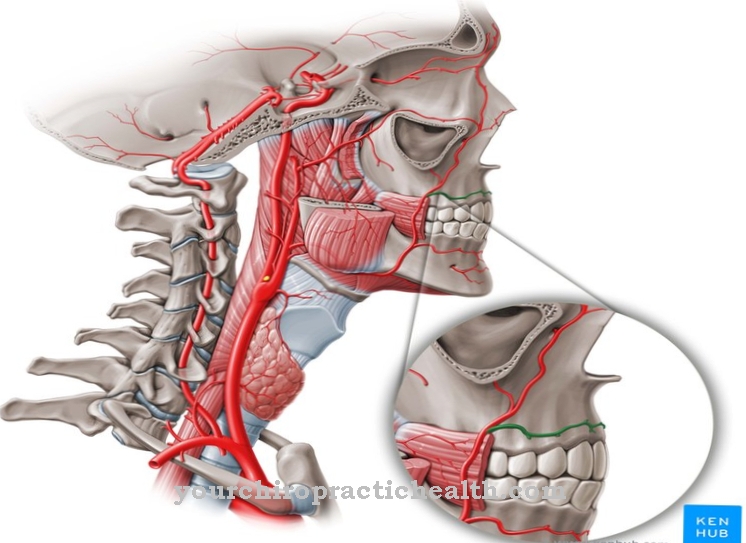
Rifampicin is administered orally. After ingestion, the antibiotic enters the blood through the intestines. Around 80 percent of it binds to plasma proteins and is evenly distributed within the organism. The highest rifampicin concentrations are reached in the bile and lungs. Two to five hours after administration, rifampicin is released from the body via the bile and stool. If the therapy lasts for a long time, this leads to a shortening of the elimination half-life.
Medical application & use
Rifampicin is mainly used against tuberculosis. This disease is caused by the Mycobacterium tuberculosis. The rifampicin-sensitive mycobacteria also include the leprosy pathogens against which rifampicin is also effective. The agent is also suitable for preventing meningitis (inflammation of the meninges) caused by meningococci. It serves to protect contact persons of the sick.
With the exception of the treatment of tuberculosis, rifampicin is not a standard antibiotic. It is often only used as a reserve antibiotic. This means that it is used when other antibiotics no longer have a positive effect due to resistance. In most cases, rifampicin is given together with an additional antibiotic. Mostly it is isoniazid.
Rifampicin is usually taken by mouth. If the patient suffers from tuberculosis, the usual daily dose is 10 milligrams of rifampicin per body weight. The agent is usually used once a day. In the case of other infections, the dosage is 6 to 8 milligrams and is given twice a day.
Risks & side effects
By using rifampicin, undesirable side effects are possible in some cases. This often leads to mild liver dysfunction. If the liver is damaged, there is a risk of serious side effects. For this reason, the doctor checks the liver functions before the therapy. It is also very important to check liver values such as liver enzymes during treatment.
In addition, when taking rifampicin, patients often experience stomach discomfort, loss of appetite, diarrhea, flatulence, nausea, vomiting, weeping reddening of the skin, itching, hives and fever. Occasionally, changes in the blood count, such as a lack of white blood cells, platelets or granulocytes, are possible. Anemia, blood clotting disorders, subcutaneous bleeding, menstrual disorders, visual disturbances, asthma-like attacks and water retention in the tissue or in the lungs are also possible. If you take rifampicin irregularly, you may experience symptoms that resemble flu.
Since rifampicin has an intense reddish-brownish color, taking the antibiotic can discolour body fluids. These include sweat, saliva, tears, and stool and urine.
If the patient is hypersensitive to rifampicin, no treatment with the antibiotic should be carried out. The same applies to pronounced liver dysfunction such as jaundice, an inflamed liver or cirrhosis of the liver and to simultaneous treatment with substances that can have a damaging effect on the liver, such as the anesthetic halothane or the mushroom preparation voriconazole. Another contraindication is treatment with HIV-1 protease inhibitors such as indinavir, saquinavir, lopinavir, atazanavir, amprenavir, fosamprenavir, tipranavir, nelfinavir or darunavir.
Treatment of acute tuberculosis with rifampicin is generally possible during pregnancy. Treatment of other diseases should, however, be done with more suitable antibiotics. There is a risk that prolonged use of the agent will lead to the inhibition of coagulation factors that are dependent on vitamin K. However, treatment during breastfeeding is not considered to be risky for the infant.




.jpg)



.jpg)